 🖨️ Print post
🖨️ Print post
When you are an excited mom-to-be, and you know that natural childbirth is important for the health of mother and child, ending up with a cesarean section (c-section) can be disappointing and even traumatic. Post-surgery, you may mourn not having a Leboyer-style gentle childbirth experience,1 or regret the baby’s missed opportunity to encounter beneficial microbes in the birth canal,2 or stew about the potentially deleterious effects of surgical birth on your infant’s brain and long-term health3,4—but it is a pretty safe bet that you are probably not thinking about how your underperforming womb contributed negatively to human evolution.5 Yet a group of theoretical biologists at the University of Vienna made headlines last year with just such a hypothesis.6
The Austria-based researchers are interested in what is known as the “obstetric dilemma,” namely the “longstanding evolutionary puzzle why the pelvis has not evolved to be wider.”6 Apparently this puzzle has been with us since the late Pleistocene era, when increasingly large-headed neonates were greeted by a pelvis previously adapted to the narrower requirements of bipedalism.7 Notwithstanding strong selection pressure, pelvic evolution seemingly never caught up to those big-brained babies. As a result, according to these researchers, the obstetric problem of “mismatched” fetal heads and maternal pelvises (called cephalopelvic disproportion or CPD) has persisted up to the present day, contributing to the sometimes life-threatening condition of obstructed labor.7
SURVIVAL OF THE UNFITTEST
Under the circumstances of overly large babies trying to ram their way through the birth canal, c-sections claim considerable credit for coming to the rescue of the beleaguered mothers. Given that obstructed labor is a frequent direct cause of maternal mortality in many lower-income countries in particular, global health experts view increased access to surgical delivery as a life-saving necessity.8 The World Health Organization (WHO) generally suggests that a country’s “ideal” c-section rate should be 10 to 15 percent, although some health researchers have suggested that high-maternal-mortality countries should set their c-section target at roughly one in five women (19 percent).9
In the United States, of course, we have gone well beyond the WHO’s modest 10 percent threshold. On average, one in three women in the U.S. currently ends up with a c-section, up from 5 percent in 1970.10 C-section rates are twice as high in older mothers (forty years or older) as they are for young mothers under age twenty, and rates rose in the over-forty age group from 30 percent in 1996 to a shocking 50 percent in 2010.11
According to the Vienna research group, the escalating c-section rate is having an “evolutionary effect.”5 Although the investigators are too polite to criticize surgical intervention, their evolutionary perspective posits that c-sections are allowing women with narrow pelvises to survive birth and “pass on their genes encoding for a narrow pelvis to their daughters,” theoretically ensuring that there will be even more c-sections in the future.5
FUNDAMENTAL LAWS OF HEALTH
Underlying the theoretical biologists’ narrative is an assumption that childbirth has always been problematic due to the basic antagonism between “neonatal encephalization” and “maternal bipedal locomotion.”12 Other researchers dispute this assumption, however, suggesting that mothers’ pelvic dimensions and fetal growth patterns are exquisitely sensitive to “ecological factors,” including diet.12 These investigators believe, therefore, in the power of nutrition to remediate maternal and perinatal mortality at least over the long term.
Back in the 1930s, an English doctor named Kathleen Olga Vaughan reached similar conclusions about the relevance of environmental influences. Dr. Vaughan extensively studied childbirth and factors associated with childbirth success or difficulty, doing first-hand research in various settings, including India, as well as extensively reviewing the scientific literature available at the time. In her fascinating volume, Safe Childbirth: The Three Essentials,13 Vaughan firmly rejected the view of difficult childbirth as “a matter of chance” or as a turn of events “dependent upon the will of Heaven,” instead asserting unequivocally that childbirth difficulties resulted from violating “the fundamental laws of health.” Far from viewing childbirth as universally dangerous, Vaughan assembled considerable evidence supporting her claim that labor is supremely uneventful when mothers-to-be are allowed to grow up in accordance with the “laws of health.” Stated another way, Vaughan argued that easy childbirth depended on “environment and the conditions in which the mother spent her childhood” [emphasis in original].
To illustrate her arguments, Vaughan’s volume offers many interesting first- and second-hand observations of sub-populations of women for whom difficult childbirth was nearly unknown. Regular readers of Wise Traditions may find it noteworthy that many of her descriptions of women experiencing easy childbirth also called attention to the excellent dental health of the women and their children. For example, boatwomen in Kashmir—who traveled with a milking goat or cow on board—“never had trouble in childbirth” and were “graceful, healthy, cheerful people, their smiling faces showing perfect teeth.” For these women, “perfect teeth, good bodily development, and intelligence [were] the rule” [emphasis in original]. In fact, Vaughan devoted half a chapter to a discussion of the teeth and jaws as indicators of “good bodily development” and especially pelvic capacity. Based on her extensive theoretical and practical experience, Vaughan concluded that perfect teeth equate to easy childbirth, while conversely there is an “essential connection between civilization, caries and difficult childbirth.”
The importance of sunlight and an active life out of doors are recurrent themes in Safe Childbirth. Commenting on Indian women living in purdah (female seclusion), Vaughan noted that the women often led a life completely devoid of sunlight, causing many to develop osteomalacia (a form of bone weakening similar to rickets). Under such circumstances, it came as no surprise that the women had abnormally high rates of difficult labor. Vaughan commented, “In all countries and districts where teeth are good, the life is an open-air one with simple food; the food, of course, varies in different places and under different conditions, but the free open-air life is a constant factor.” Reinforcing the relevance of environmental factors, Vaughan also observed that easy and difficult childbirth might coexist within the same country, race or even family and that lifestyle was the determining factor: “Easy childbirth characterizes those living an outdoor life while difficulty is the portion of those living indoors from infancy, confined there by social or educational tyranny.”
In one chapter, Vaughan drew from an ethnography called The Maori to illustrate the tragic transition from easier to more difficult childbirth that she and others such as Dr. Weston A. Price started witnessing in their era. The author of that work (New Zealand ethnographer Elsdon Best) remarked: “Children from 6 to 12 years used to run about naked and their teeth were perfect. Now the teeth begin to decay, the race suffers from consumption, and there is also trouble in childbirth.” Best attributed the problems with childbirth to “the adoption of European medicines, food, and clothing.”
THE THREE ESSENTIALS
Vaughan’s research distilled “three essentials” of easy childbirth: a round pelvic brim, flexible joints and natural posture. With regard to the first, Vaughan identified several reasons why a round or circular pelvic brim facilitates easy labor. First, a round brim offers the self-evident advantage of making everything roomier. Second, the round brim “matches the halo measure [circumference] of the fetal head, so that they fit as a cup and ball fit one another.” Just as important, the round brim “always co-exists with a well-shaped outlet,” which offers the baby easier passage through the birth canal.
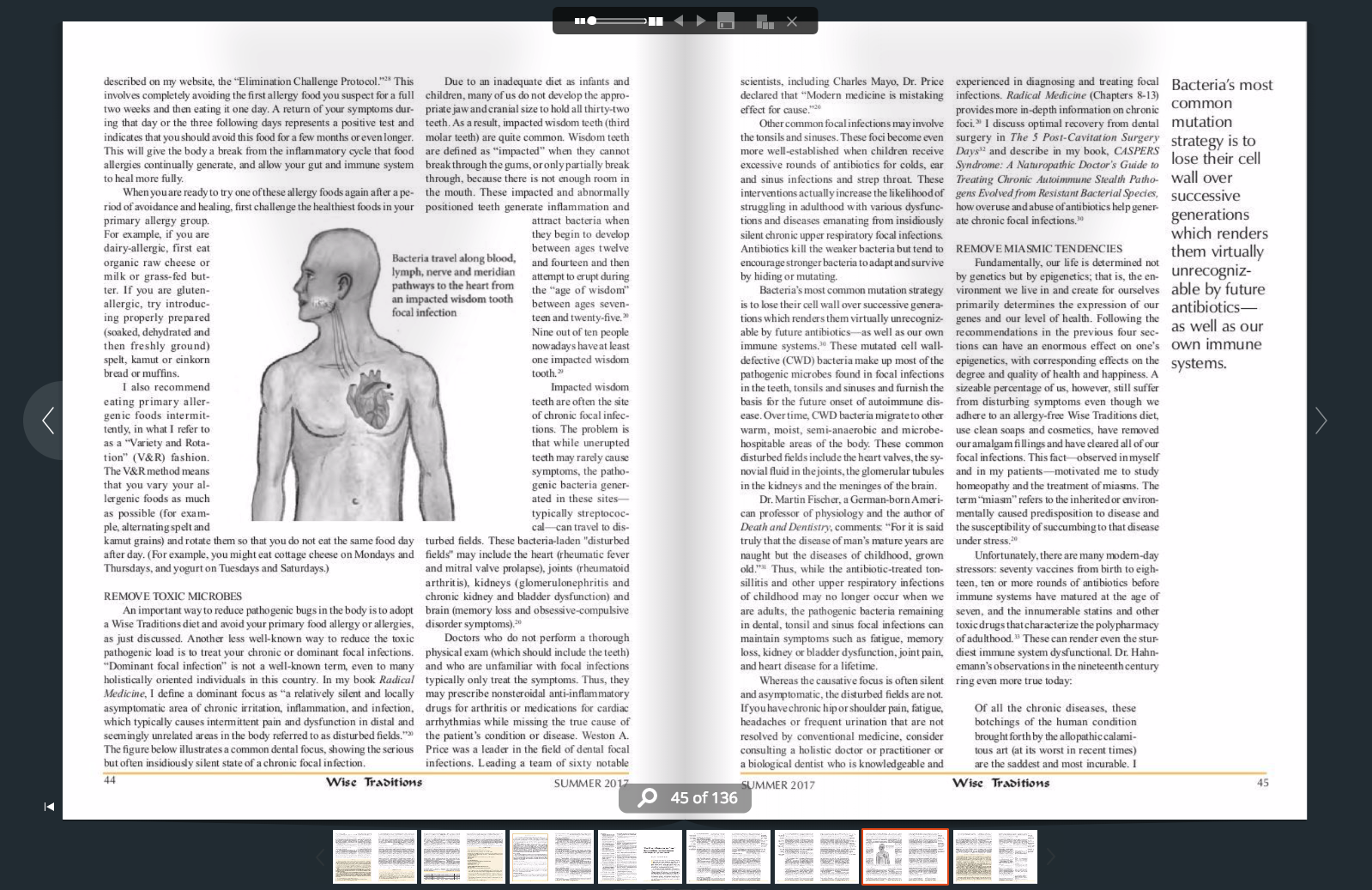
Unfortunately, Vaughan observed that a trend toward an oval rather than circular brim had accompanied the advances of “civilization.” In a simple but compelling illustration (Figure 1), Vaughan noted that the circle and oval have the same circumference, but the oval has less area and causes more difficulties during childbirth. Vaughan then asked her readers to consider why this “strange metamorphosis” from round to oval occurs. It turns out that the other two “essentials” have something to do with it. For example, mobile pelvic joints play a key role in the development of normal pelvic shape. Vaughan cited a researcher who believed that “much backache and suffering which women endure might be entirely avoided if young and growing female children were made to do exercises in the prone position at school, such as crawling exercises—to keep the sacro-iliac joints supple—which will be of such value to them when they reach the child-bearing age.”
Drawing on anthropological evidence, Vaughan also pointed out the especially critical role of posture, the third “essential.” Anyone who has contemplated the superb photos in Esther Gokhale’s book, 8 Steps to a Pain-Free Back,14 will understand Vaughan’s statement that “posture and posture alone can cause modifications in the skeleton of a person in perfect health.” Vaughan noted that habits such as sitting for long hours at school could bring about undesirable changes in structure.

Vaughan emphasized that the pelvis is the most rapidly growing part of the whole body, but particularly during the crucial preadolescent and early adolescent years. Vaughan’s discussion of osteomalacia has great relevance for the young girls of today, because Vaughan believed that weak bones were entirely preventable. Vaughan reached the conclusion that the “crumpled” pelvic shape characteristic of osteomalacia was “entirely attributable to factors operative in the patient’s own lifetime”—and especially to “conditions prevailing before puberty” [emphasis in original].
Given that many people are currently returning to an awareness of the pivotal importance of sunlight for good health,15,16 Vaughan’s prescription for heliotherapy and her beliefs about sunlight’s central role are quite intriguing. In short, Vaughan believed that “difficult childbirth either in the East or the West is caused by faulty pelvic development due to want of sufficient light on the skin during the years preceding puberty.”
NEW CHALLENGES
In recent years, there has been an appalling increase in maternal mortality in the US, making it an outlier among rich nations.17 Over the eighteen-year period from 1990 to 2008, maternal mortality doubled, giving the US the unimpressive rank of fiftieth in the world.18 According to Ina May Gaskin, famed author of Spiritual Midwifery, the maternal death ratio (number of maternal deaths per hundred thousand births) “is almost five times as high as it should be” for all American women, and “more than ten times what it should be” for African American women.19
In purely economic terms, women’s health advocates note that “for a country that spends more than any other country on health care and more on childbirth-related care than any other area of hospitalization…this is a shockingly poor return on investment.”18 The trend also gives special meaning to Vaughan’s macro-level observation that “the number of women who die in childbirth [is] a rough index to the rate at which any nation is going downhill.”
The increase in maternal mortality has been driven, in part, by the explosion of chronic medical conditions such as diabetes, obesity and heart disease.20 The head of the Centers for Disease Control and Prevention’s Maternal and Infant Health Branch has commented, “The really scary thing to us is all the deaths from cardiovascular disease and heart failure,” noting that these represent fully one-fourth of all maternal deaths.20
Many of these chronic ailments also increase a woman’s chances of ending up with a c-section. For example, obesity is a known risk factor for surgical delivery.21 Given that failure to progress and CPD are among the top indications for cesarean deliveries in young women under the age of twenty-five,11 it is discouraging to note that c-section rates for both of these two indications also increase markedly with level of obesity.22
Further, c-sections increase the risk of life-threatening complications in and of themselves.23 For example, cesarean delivery nearly doubles a pregnant woman’s risk for thromboembolism (blood clots), another leading cause of maternal deaths in the US.24 A Scandinavian study found that c-sections were associated with an elevated risk of a thromboembolic event for as long as one hundred and eighty days postpartum, which is well beyond the six weeks typically defined as the postpartum period.25
RECLAIMING CHILDBIRTH
Overall, the Vienna researchers’ claims seem strangely oblivious to the role of nutrient-dense diets and other important lifestyle factors that powerfully shape the health and childbirth outcomes of mothers-to-be. This does not mean that we are going down a blind alley, however, when we consider the implications of so many c-sections. Belatedly, other investigators are pointing out the need to examine both the risks and benefits of cesarean delivery, particularly since research is uncovering a much higher incidence of chronic diseases (including asthma, obesity and type 1 diabetes) in children born via c-section.4 If c-section babies are indeed missing out on maternal microbiome exposure—as well as brain stimulation, important early bonding and probably many other as-yet-unidentified but irreplaceable aspects of natural childbirth—then we may indeed be setting transgenerational (or epigenetic) changes into motion. What will happen when a sizeable proportion of the population has a hospital-generated microbiome? It is only slightly reassuring to hear that the Austrian researchers do not believe that non-surgical births will become fully “obsolete.”5
SIDEBARS
DR. VAUGHAN AND DR. PRICE
Not surprisingly, Dr. Weston A. Price was aware of Dr. Vaughan’s work. In Nutrition and Physical Degeneration, Dr. Price recommended that Safe Childbirth “be made available for reference in the school libraries of the United States.” Discussing the generational changes that were beginning to occur with the transition away from nutrient-dense foods, Dr. Price remarked, “I am informed by gynecologists that narrowing of the pelvic arch is one of the factors that is contributing to the increased difficulties that are encountered in childbirth by our modern generation.” Dr. Price concurred with Dr. Vaughan that “method of life” and nutrition are key determinants of proper structure and function for future parents.
CAN THIS BE NORMAL?
The dismal childbirth trends that we observe today were already well under way in Dr. Vaughan’s time. Vaughan quoted a leading work on obstetrics from the 1930s by Joseph De Lee: “Is labor in the woman of today a normal function? I say it should be, but it is not. Can a function so perilous that, in spite of the best care, it kills thousands of women every year, that leaves a quarter of the women more or less invalided, and the majority with permanent anatomic changes of structure, that is always attended by severe pain and tearing of tissues, and that kills 3 to 5 percent of children—can such a function be called normal?”13 Vaughan herself described the “bruising and tearing of soft parts, the exhaustion of the mother, the risk of sepsis and of puerperal fever, all conditions directly due to this primary failure of adaptation between mother and child which lengthens out the natural process of birth into many hours, or even days.”
Vaughan’s book offers numerous descriptions of uncomplicated childbirth taking place in natural settings without distress. In contrast, modern hospital-based birth has become a highly controlled and frequently disempowering experience: “The intravenous [IV] drips commonly attached to the hands or arms of birthing women make a powerful symbolic statement: [the drips] are umbilical cords to the hospital. By making her dependent on the institution for her life, the IV conveys to her one of the most profound messages of her initiation experience: in the contemporary American technocracy, we are all dependent on institutions for our lives, ‘umbilically’ linked to them through the water and sewer pipes, electrical wires, and TVs that pervade our homes, through our banking accounts and credit cards, and increasingly through our laptops, cell phones, iPads, and the like. The rituals of hospital birth are not accidental—they are profound symbolic and metaphoric expressions of technocratic life.”26
REFERENCES
1. Leboyer F. Birth without Violence. New York, NY: Alfred Knopf; 1975.
2. Handwerk B. Does having a c-section alter baby’s first microbiome? Smithsonian.com, February 1, 2016.
3. Peart KN. Natural birth—but not c-section—triggers brain boosting proteins. Yale News, August 8, 2012.
4. Blustein J, Liu J. Time to consider the risks of caesarean delivery for long term child health. BMJ 2015;350: h2410.
5. Briggs H. Caesarean births “affecting human evolution.” BBC News, December 7, 2016. http://www.bbc.com/news/science-environment-38210837.
6. Mitteroecker P, Huttegger SM, Fischer B, et al. Cliff-edge model of obstetric selection in humans. PNAS 2016;113(51): 14680-5.
7. Fischer B, Mitteroecker P. Covariation between human pelvis shape, stature, and head size alleviates the obstetric dilemma. PNAS 2015;112(18): 5655-60.
8. Harrison MS, Griffin JB, McClure EM, Jones B, Moran K, Goldenberg RL. Maternal mortality from obstructed labor: a MANDATE analysis of the ability of technology to save lives in Sub-Saharan Africa. Am J Perinatol 2016;33(9):873-81.
9. Molina G, Weiser TG, Lipsitz SR, et al. Relationship between Caesarean delivery rate and maternal and neonatal mortality. JAMA 2015;314(21): 2263-70.
10. Lake N. Labor, interrupted. Cesareans, “cascading interventions,” and finding a sense of balance. Harvard Magazine, Nov/Dec 2012.
11. Timofeev J, Reddy UM, Huang CC, Driggers RW, Landy HJ, Laughon SK. Obstetric complications, neonatal morbidity, and indications for cesarean delivery by maternal age. Obstet Gynecol 2013;122(6): 1184-95.
12. Wells JCK, DeSilva JM, Stock JT. The obstetric dilemma: an ancient game of Russian roulette, or a variable dilemma sensitive to ecology? Am J Phys Anthropol 2012;149(S55).
13. Vaughan, Kathleen Olga. Safe Childbirth: The Three Essentials. Round Brim, Flexible Joints, Natural Posture. London: Baillière, Tindall and Cox; 1937.
14. Gokhale E. 8 Steps to a Pain-Free Back: Natural Posture Solutions for Pain in the Back, Neck, Shoulder, Hip, Knee, and Foot. Pendo Press; 2008.
15. Seneff S. Sulfur deficiency: a possible contributing factor in obesity, heart disease, Alzheimer’s and chronic fatigue. Wise Traditions 2011;12(2): 17-28.
16. Hernandez C. Heliotherapy: benefits of the sun far and beyond vitamin D. http://www.thehealthyhomeeconomist.com/heliotherapy-benefits-of-the-sun-beyond-vitamin-d/.
17. MacDorman MF, Declercq E, Cabral H, Morton C. Recent increases in the U.S. maternal mortality rate: disentangling trends from measurement issues. Obstet Gynecol 2016;128(3):447-55.
18. Coeytaux F, Bingham D, Strauss N. Maternal mortality in the United States: a human rights failure. Contraception 2011;83:189-193.
19. Gaskin IM. Maternal death in the United States: a problem solved or a problem ignored? J Perinat Educ 2008;17(2): 9-13.
20. Tavernise S. Maternal mortality rate in U.S. rises, defying global trend, study finds. The New York Times, Sept. 21, 2016.
21. Bautista-Castaño I, Henriquez-Sanchez P, Alemán-Perez N, Garcia-Salvador JJ, Gonzalez-Quesada A, Garcia-Hernandez JA, Serra-Majem L. Maternal obesity in early pregnancy and risk of adverse outcomes. PLoS One 2013;8(11): e80410.
22. Kawakita T, Reddy UM, Landy HJ, Iqbal SN, Huang CC, Grantz KL. Indications for primary cesarean delivery relative to body mass index. Am J Obstet Gynecol 2016;215(4): 515.e1-9.
23. Martin N, Montagne R. Focus on infants during childbirth leaves U.S. moms in danger. NPR, May 12, 2017.
24. American College of Obstetricians and Gynecologists. New recommendations to prevent blood clots during Cesarean deliveries issued. August 22, 2011.
25. Galambosi PJ, Gissler M, Kaaja RJ, Ulander VM. Incidence and risk factors of venous thromboembolism during postpartum period: a population-based cohort-study. Acta Obstet Gynecol Scand 2017 Mar 30.
26. David-Floyd RE. The rituals of American hospital birth. Global Freedom Movement, February 6, 2015.
This article appeared in Wise Traditions in Food, Farming and the Healing Arts, the quarterly magazine of the Weston A. Price Foundation, Summer 2017.
🖨️ Print post

Leave a Reply