 🖨️ Print post
🖨️ Print post
How Your Gallbladder Can Sabotage Your Weight, Emotions, Food Plan and Life!
Casey, age forty-one, slumped in the consulting room chair. Her skin was rough and coarse, with shadows under her eyes. Her breath was often sour, as was her general attitude about life. Her twenty pounds of extra fat were centered uncomfortably around her belly and hips.
“Can’t you help me, doctor? It feels like my body is betraying me. All I want to do is eat sweets! I have tried and tried to diet and exercise, but sooner or later I cheat and eat sugar! I wake up with a sour stomach every day and can’t even eat until hours later. I have so much gas and burping. I know I’m supposed to eat this great grass-fed butter and take cod liver oil every day, but I get stomach cramps when I eat anything fatty and even the smell of them makes me nauseous. I make bacon and eggs for the kids’ breakfast, but I just eat toast or have tea—and I still keep gaining weight! My skin is aging and I have hard white bumps on the backs of my arms. And I can’t even stand to be in the same room with my husband and kids for long. I love them, but I am so irritated by them that I just want to go into my bedroom and lock the door so I don’t snap at them. What is wrong with me?”
I see a “Casey” in my practice almost every day. Why? The answer has to do with the liver and its trusty but sometimes tricky sidekick, the gallbladder. Unfortunately, gallbladder problems can affect every aspect of a person’s life, including food choices, weight, mineral absorption, hormone balance, emotional balance, family dynamics and intimate relationships. I’ve seen divorces related to faulty gallbladder function, even involving otherwise wonderful people!
THE ALL IMPORTANT LIVER
The liver—which traditional Chinese medicine views as the seat of emotion and intelligence1—is a miraculous organ with an unbelievable number of functions. I am going to focus on just two aspects of this organ: fat digestion and hormone management. Both of these functions are incredibly important in determining how we feel and what we can successfully eat.
A healthy liver produces over a quart of bile daily, which is supposed to be a thin, slippery, yellowish alkaline enzyme complex that breaks down fats for absorption in the small intestine. However, a variety of conditions can set the stage for bile to change into a thicker, stickier, creamier and more acidic fluid. Further metabolic problems (often related to stress and resultant low stomach acid production) and nutritional deficiencies (including deficiencies of vitamin A, lecithin, choline, methionine and essential fatty acids) can cause the bile ducts to contract poorly so that the bile is retained too long in the liver and gallbladder. When this happens, the bile will congeal, forming a “sandy” or “gravel-like” sludge made of cholesterol and bile salts—and eventually forming hard and sometimes mineral-based gallstones and liver stones.2 These stones further limit bile flow and therefore reduce fat digestion, causing the fat in food to sit around in the stomach and small intestine and basically go rancid. Problems with bile production also impair some of bile’s other important roles, including removing fat-soluble toxins from the body and preventing the development of food allergies.
Congested bile has also long been known to have emotional repercussions, including causing irritability. In fact, the terms “choleric,” “melancholic” or “of a bilious nature” have been used to refer to an irritable, moody or angry person in writings even from before the time of Christ.
CAUSES OF GALLBLADDER DYSFUNCTION
Although classic medical gallbladder cases are inelegantly said to be “4F”—female, fertile, fat and forty—the problem is occurring in ever younger people of both genders, in large part due to our increasingly toxic foods and lifestyles.
Low (not high!) stomach acid is a primary direct cause of “liver congestion” and gallbladder dysfunction, but there are a number of other risk factors. These include dietary factors such as diets high in simple carbohydrates, low in fiber, low in traditional fats or high in “fake fats” such as margarine; excessive protein intake; overconsumption of fried foods; a history of a vegetarian or vegan diet; deficiencies of phosphorous and magnesium (related to calcium stone formation); low dietary choline, methionine and/or lecithin (common in those who avoid egg yolks); and overeating or obesity.3 There are also medication-related risk factors,4 including a history of use of birth control pills (women), synthetic hormones or statin drugs. Women with high estrogen levels (estrogen dominance) are particularly prone to gallbladder problems and the emotional chaos that results. Individuals with symptoms or lab results indicative of hypothyroidism5 or a history of chronic dehydration also can be at risk of gallbladder dysfunction, as can those with lifestyles high in stress or anger-creating situations.
THE WISDOM OF THE “FAULTY” BODY
Here is why Casey does not like to eat her grass-fed butter and bacon: her body is wise. It knows that it cannot properly digest that fat, and it does not want to add removal of rancid fat to its burden. As a result of this bodily wisdom, Casey gets the message from her gut not to eat these otherwise healthy foods. This can appear as either nausea, not feeling hungry (especially in the morning) or having strong cravings for carbohydrates (because she can still digest those—for now). Inability to digest fats is a primary reason for sugar and carbohydrate cravings, making mood and weight stability very challenging.
In a vicious cycle, once Casey stops digesting fats well, not only will she develop an aversion to good fats and proteins, but the fat-soluble vitamins (the noble vitamins A, D, E and K) will pass right through her bowels as well. Unfortunately, she needs those fat-soluble vitamins for myriad reasons, one of which is (you guessed it) proper liver and gallbladder function!
SIGNS AND SYMPTOMS
The signs and symptoms of gallbladder problems are many and diverse, and range from mild to incapacitating (see below).
Severe or advanced gallbladder inflammation (cholecystitis) can lead to sharp, urgent pain on the right side (often felt as a sharp band of pain around the middle) and/or pain in the midshoulder blade area that can be severe enough to lead to an emergency room (ER) visit. These pains may come and go, depending on diet and stress levels.
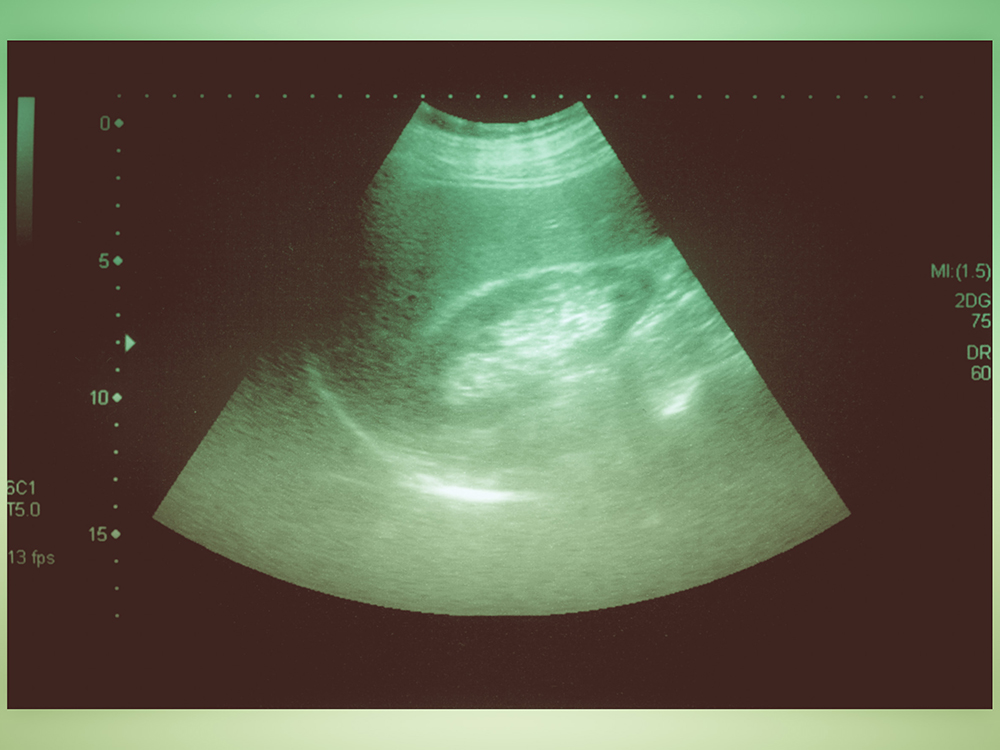
DIAGNOSING GALLBLADDER PROBLEMS
Imaging (such as an x-ray) often misses gallbladder congestion issues, as many gallstone symptoms are caused by thickened bile, not mineral-based stones. Unfortunately, the modern set of typical lab tests also can easily miss a chronic gallbladder problem. This can lead practitioners astray if they are “treating by paper” (lab results) rather than “treating by patient” (signs, symptoms and physical exam). Standard lab tests are valuable for indicating whether there is another problem in the area, such as an infection, but only sometimes—and not always—can they point to liver and gallbladder stasis (congestion). Tests include a complete blood count (CBC) as well as tests to assess levels of bilirubin (a marker of liver function), albumin (a protein made by the liver) and various enzymes: ALP (alkaline phosphatase), AST/SGOT (aspartate aminotransferase/serum glutamic-oxaloacetic transaminase) and GGT (gamma-glutamyl transferase). It also may be wise to run some thyroid tests—thyroid-stimulating hormone (TSH), free T3, reverse T3 and free T4—because low thyroid function is a significant factor in gallbladder issues.
During the medical visit, it is prudent to ask for an abdominal exam, which should include palpation of the gallbladder reflex point (midright rib border) and a “Murphy’s Sign” test (also called a “Murphy’s Rebound” test). With the latter, pain or tenderness in the gallbladder area gets worse after the pressure is abruptly removed (that is, the “rebound” pain is worse than the direct pressure pain). This usually means trouble. An oral pH test can also be a good idea; a pH of under 7-7.2 can be related to low stomach enzyme production, low fat absorption and subsequent low bile output. Primarily, however, diagnosis of gallbladder problems should be based on what patients tell their doctors—not on which tests are ordered.
CONVENTIONAL TREATMENT
When a serious gallbladder problem is diagnosed, the usual medical solution (undergone by over half a million Americans per year) is surgical removal of the gallbladder; other “standard” medical treatments (such as drugs and a procedure involving high energy shock waves called lithotripsy) are not very effective. Typically, practitioners carry out gallbladder surgery via laparoscope, considered easier on the patient. Unfortunately, laparoscopic gallbladder surgery has a dramatically increased rate of damage to the bile ducts6 as well as other complications.7
In addition, gallbladder surgery sets patients up for a lifetime of reduced ability to digest fat (while failing to improve mortality rates from gallbladder disease) because the ongoing “liver congestion” problem continues. Thick, sludgy bile continues to get stuck in the liver, resulting in ongoing digestive problems, fussy eating and pain in the liver area. Those who have had gallbladder surgery are not, therefore, off the hook for dealing with this problem! In fact, people who have had gallbladder surgery should consider taking a bile-based digestive enzyme—for life—with any meal that contains fat, because they cannot effectively store and release enough bile at the proper times.
THREE COMMON SENSE THERAPIES
Naturopathic physicians equate the surgical solution to removing the light bulb of the “check engine” light on a car dashboard rather than repairing the engine. Fortunately, there is a better way. It is possible to combine good lifestyle habits and common sense therapies into effective prevention and rehabilitation of gallbladder problems. Ironically, parts of the very best prevention—a Wise Traditions diet—can be intolerable in the short term for those who have serious gallbladder problems. Like Casey, those with gallbladder issues often exhibit significant fat or meat intolerance, indigestion or aversion, making some of the Weston Price dietary guidelines frustrating to follow. Rather than avoiding good healthy fats over the long term, those folks need serious, educated help to rehabilitate the gallbladder and liver safely.
There are three simple and safe things that everyone can do to help support the gallbladder. (See sidebars for other safe and effective measures for both prevention and treatment.) As an important first step, one should consider the various factors (listed earlier) that commonly contribute to liver and gallbladder problems and strive to eliminate or reverse them.
A second easy step is to consume real, naturally fermented apple cider vinegar. There are several reasons why this old folk medicine standby helps. First, it lowers the pH of the stomach contents, which helps gently trigger bile release with food. It also contains malic acid and phosphorous, which help slowly thin bile. Finally, real apple cider vinegar contains good probiotics. I suggest taking two teaspoons in an ounce of water before meals. Honey is optional. If apple cider vinegar causes any concerns such as stomach pain, a visit to a holistic physician is important, as there could be an underlying stomach condition such as an ulcer.
A third simple action is to make sure that the diet includes beets in all their glory (see recipe). Beets are liver and gallbladder allies in many ways. They contain helpful minerals, amino acids, galacturonic acid, lactulose and a variety of organic acids that help thin bile, such as citric, malic, tartaric and malonic acids and others.
BACK TO BUTTER
What happened to Casey? Fortunately, Casey is a member of the Weston A. Price Foundation! Because fats (in the short term) were making her worse, she went on a temporary high-vegetable and lowfat food program. She was able to follow the rest of the WAPF dietary guidelines (increasing broth-based soups and eating some fruit, fish, properly prepared whole grains and homemade kefir). She also stopped taking oral contraceptives, halted her statin drug, ate beet salads (see recipe in sidebar) and started taking apple cider vinegar before each meal. After one week, she felt better and was able to test and then correct her low stomach acid levels. She also went through a gentle liver and gallbladder detox program. Casey now enjoys grass-fed butter and bacon with the rest of the family, and her marriage is better, too!
REFERENCES
1. The emotions. https://www.chinesemedicineliving.com/philosophy/the-emotions/.
2. Hill PA, Harris RD. Clinical importance and natural history of biliary sludge in outpatients. J Ultrasound Med 2016;35(3):605-610.
3. Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver 2012;6(2):172-187.
4. Chatterjee S, Annaert P. Drug-induced cholestasis: mechanisms, models, and markers. Curr Drug Metab 2018 Apr 27. doi: 10.2174/1389200219666180427165035. [Epub ahead of print.]
5. Inkinen J, Sand J, Nordback I. Association between common bile duct stones and treated hypothyroidism. Hepatogastroenterology 2000; 47(34):919-921.
6. Hogan NM, Dorcaratto D, Hogan AM, et al. Iatrogenic common bile duct injuries: increasing complexity in the laparoscopic era: a prospective cohort study. Int J Surg 2016;33(Pt A):151-156.
7. Alexander HC, Bartlett AS, Wells CI, et al. Reporting of complications after laparoscopic cholecystectomy: a systematic review. HPB (Oxford) 2018 Apr 9. pii: S1365-182X(18)30779-2. doi: 10.1016/j.hpb.2018.03.004. [Epub ahead of print]
8. Einarsson K, Nilsell K, Leijd B, Angelin B. Influence of age on secretion of cholesterol and synthesis of bile acids by the liver. New Engl J Med 1985;313(5):277-282.
9. Dr. Page’s food plan: supporting whole food nutrition. International Foundation for Nutrition and Health. http://ifnh.org/dr-pages-food-plan/.
10. Pendick D. How much protein do you need every day? Harvard Health Blog, June 18, 2015. https://www.health.harvard.edu/blog/how-much-protein-do-you-need-everyday-201506188096.
SIDEBARS
SIGNS AND SYMPTOMS OF GALLBLADDER PROBLEMS
Gallbladder troubles may include some (or many) of the following signs and symptoms:
• MOOD: irritability, anxiety and/or moodiness (traditionally “melancholy”).
• ENERGY: insomnia, fatigue.
• CRAVINGS: persistent sugar or carbohydrate cravings.
• AVERSIONS: fat or protein avoidance or intolerance; side pain or shoulder blade area pain, aversion, belching or nausea after eating eggs, dairy, onions, pork (especially bacon), chocolate, corn, citrus, beans, nuts, processed foods or any fats.
• DIGESTION: burping after meals, gas, bloating, reflux/gastroesophageal reflux disease (GERD).
• ELIMINATION: light-colored, clay-like or pasty stools that may come and go; stools that float; diarrhea (especially diarrhea that changes with the fat content of the diet); alternating diarrhea and constipation.
• WEIGHT: persistent obesity.
• SKIN: fat-soluble vitamin deficiency symptoms like persistent white “bumps” on the outer upper arms or around the eyes; thick callouses on the heels; dry skin.
• FOOD ALLERGIES
• THYROID PROBLEMS
• OTHER: shadows under eyes, bad breath (especially after fatty meals), thick coating on tongue, suboptimal cholesterol ratios.
LOVE YOUR LIVER AND GALLBLADDER: PREVENTION AND SAFE INTERVENTION
There are many safe and effective dietary and lifestyle steps that one can take to support the liver and gallbladder and prevent gallbladder issues:
1. NOT OVEREATING: It is important to avoid overeating, particularly in the evenings after 6:00 pm when bile flow is naturally at its lowest. Most people digest optimally a meal size of about two (of their own) cupped hands full of food per meal. Older folks often do well with two meals a day rather than three. Sticking to two to three meals a day—with no snacks—helps create the proper pH and transit time in the intestine.
2. GOOD FATS: Most of us need a minimum of about ten grams (two teaspoons) of good fat per meal (ninety calories worth) to stimulate the gallbladder to release bile. However, if fat consumption causes nausea, abdominal pain, rightsided discomfort, diarrhea or pain around the shoulder blades, it’s time to seek medical care.
3. STOMACH ACID: It is the pH of the stomach contents that triggers the message to the gallbladder to contract and release bile, so low stomach acid is a set-up for low bile flow. Avoid antacid drugs but recognize that low stomach acid is very common after prolonged stress or stressful events and as a feature of aging.8 A person whose doctor does not know how to check stomach acid carefully should find a knowledgeable functional, integrative or naturopathic doctor.
4. DIETARY AND OTHER RISK FACTORS: Cut down on sugar, processed foods, fried foods, vegetable oils and trans fats as well as drugs and stress.
5. PROTEIN INTAKE: Protein is critical, but consuming much more than one needs or can digest causes multiple problems. Unfortunately, guides for protein intake are all over the map and require tailoring to the individual. For example, one guide for adults recommends dividing one’s “ideal body weight” by fifteen to ascertain the number of ounces of protein needed in a day.9 Some medical guidelines recommend multiplying one’s weight (in pounds) by 0.36 to get grams of protein per day.10 (A more specific protein calculator is available on my website, vitalitymedicine.org.)
6. WEIGHT: Avoid fad and yo-yo dieting or rapid weight loss (and regain). Slow and steady weight loss (if needed) helps the most.
7. SALT: Don’t skip the salt. We need salt (chloride) to make stomach acid. Sea salt is the ideal type of salt to consume.
8. “LIVER TONIC” FOODS: It is helpful to increase one’s intake of beets, beet greens, artichokes, burdock, fennel, parsley, cilantro, salad dressings containing lemon juice or vinegar, high-fiber foods and fermented foods. Vegetable fiber helps bind and pull “toxic” bile out rather than having it recycle back to the liver.
9. BOWELS: Treat constipation seriously. A healthy person should have one to three bowel movements a day.
10. HYDRATION: It is important to hydrate well. “Sticky” blood and thick bile do not work well.
MORE ASSERTIVE INTERVENTIONS FOR GALLBLADDER ISSUES
There are additional interventions that can help with gallbladder issues. However, those with acute pain or significant gallstones should consult a physician before undertaking any of these more active interventions so as not to provoke or exacerbate the problem. An intervention that someone is not personally ready for can trigger a healing crisis.
1. INTERMITTENT FASTING: This can be very helpful and can be as simple as skipping dinner or breakfast one to three times a week and replacing the meals with fresh vegetable juice or skimmed bone broth to “rest” the digestive system. Many traditional cultures incorporated some kind of fasting as an important element of their religion, customs or lifestyle. To adopt aspects of traditional diets without acknowledging and incorporating the fasting component is a set-up for conditions of “excess” such as obesity and cholestasis (problems with bile flow). Pregnant women should not fast.
2. BITTERS: Pre-digestive tonics are popular in many cultures and include angostura bitters, bitter or sour aperitifs, bitter salads and Swedish bitter herbal tinctures and teas. These bitter flavors stimulate healthy stomach acid production and healthy bile flow.
3. LIVER TONIC HERBS: Safe herbs for most (non-pregnant) folks include dandelion root, burdock, berberine (Oregon grape root), artichoke (Cynara scolymus) and milk thistle (Silybum marianum). Peppermint, chamomile and fennel, gentle herbs that support stomach and liver function (such as in tea), are generally recognized to be safe during pregnancy.
4. MINERAL DEFICIENCIES: Deficiencies of key minerals such as magnesium should be corrected.
5. CLEANSES: There are many forms of liver cleanses or “spring cleanses” out there (and it is beyond the scope of this
article to describe them all). Traditionally, European and American medicine included a cleanse in the spring that involved a combination of fasting and/or vegetarian fare, bitter herbs, laxative herbs, castor oil packs on the liver, saunas or sweats, movement therapy, sunbathing, colon hydrotherapy (such as coffee enemas) and local or whole-body contrast hydrotherapy (see #6). However, cleansing should not be adopted as a “lifestyle”; that is, cleansing strategies (such as a juice fast or temporary vegetarian diet) can work well in the short term but should not be continued indefinitely or other imbalances will occur. Working with an experienced healer is ideal to help create a cleanse that fits each person’s individual needs. Pregnant and nursing women should not do cleanses.
6. CONTRAST HYDROTHERAPY: Contrast hydrotherapy, an ancient technique that moves stagnant fluids, is a technique that fits almost everyone. It can be used in one area (such as over the liver) or as a whole-body treatment (such as in the bath or shower). To start, simply immerse (or put a hot pack on) the liver area—as hot as is comfortable—for three minutes; then change to cold water or an ice pack—as cold as one can tolerate—for thirty seconds. Repeat three times and be sure to always end with cold. If carried out correctly, one should feel invigorated, not chilled!
7. OLIVE OIL FLUSHES: Olive oil flushes have become somewhat famous—or infamous. A casual Internet search for gallbladder issues will uncover endless variations of this old standby for flushing “stones” out of the gallbladder. Most of the “stones” flushed are actually not stones but a congealed mix of cholesterol and bile purged from the liver and gallbladder, mixed with the olive oil. Although the procedure does not flush actual stones, it does remove some bile that would otherwise recirculate. Conventional doctors consider olive oil flushes as dangerous heresy because of the theoretically possible risk of flushing a stone into the bile duct and causing an impaction (which would be a medical emergency). I have never seen a case of this in my twenty-five years of practice, but I do not usually recommend olive oil flushes as a first-line therapy without adequate medical support, in part because of the possible risk of impaction. Other reasons that I do not typically encourage them include the potential for nausea from the big quaff of olive oil and the basic fact that more prudent actions are often enough to make lasting improvements. Individuals who choose an olive oil flush should be cautious and seek the help of a physician to make sure it is safe. Individuals likely to have active gallstones or an infection (such as those with a positive Murphy’s Sign test) should not do an olive oil flush!
BEET SALAD TO SUPPORT THE LIVER AND GALLBLADDER
The following recipe is for a tasty liver and gallbladder tonic food that is appropriate for most people.
• 4 cups shredded beets
• 2-4 cups beet greens, steamed and chopped
• 2 cups shredded carrots (optional)
• 1/3 cup vinegar or lemon juice
• Olive oil (to taste)
• Garlic to taste (optional)
• Freshly grated ginger to taste (optional)
• Sea salt and pepper
Clean and shred the fresh beets and optional carrots. Combine beets, carrots and beet greens with vinegar or lemon juice and add olive oil to taste (if fats are tolerated). Add optional garlic and ginger, sea salt and pepper to taste. Let mixture rest in the fridge for an hour, stir and eat. Keeps for one week in the fridge.
This article appeared in Wise Traditions in Food, Farming and the Healing Arts, the quarterly magazine of the Weston A. Price Foundation, Summer 2018.
🖨️ Print post

Oh my gosh, I could cry reading this, it gives me so much hope and encouragement. I am pregnant and was told that I will likely need to have my gallbladder removed after the baby is born, but I really felt there must be a better way. And what repercussions could their be from removing it? I wanted more answers and it didn’t seem like there were any answers! I was also feeling stuck because I have been trying to incorporate the WAPF diet into my family’s life for the last three of four years and was beside myself when I was told to eat a low-fat diet! Of course I have to for the time being, but this article gives me such a wonderful start and I think I am going to try to find a naturopathic doctor in my area to see if we can improve this gallbladder of mine.
Such a fantastic article. I’ve done so much research and learned a lot on my own but this really covers almost all of it. I wish more people could read this before having their GB removed or allowing their issues to progress to a lot of pain.
Diet/nutritional recommendations for those who have already had their gallbladder removed?
The most solid resonating advice ever thank you! Although difficult to understand if you are only dealing with mild symptoms and have no support. My summary is eat an EXTREMELY gentle version of the typical wise traditions diet and follow your instincts while also promoting recycling and regeneration via detox cleanses and fasts.
Thankful I wasn’t experiencing severe intolerance… y’all are in my thoughts and prayers. Treat your thyroid like it’s on low battery. No stress. Send those around you snippets of this page to help them understand. <3