 🖨️ Print post
🖨️ Print post
Translations: Spanish
An Introduction to the Major Hormones that Operate and Maintain the Body
Life is a continuum of constant change. The body, the vessel that houses us in the course of life’s journey, is in a constant state of adaptation and adjustment. In addition to the changes from conception, birth and childhood, puberty, to maturity, senescence and death, the body has diurnal and seasonal rhythms, as well as others with cosmic forces far beyond our present earthly cognizance. It responds to stimuli and interactions with the external environment as well as to fluctuations and changes within itself.
Reception and response to external stimuli connect us with the world around us. Internal processing of such input serves to shape and clarify who we are, how we interact with the world, and what we give back to it.
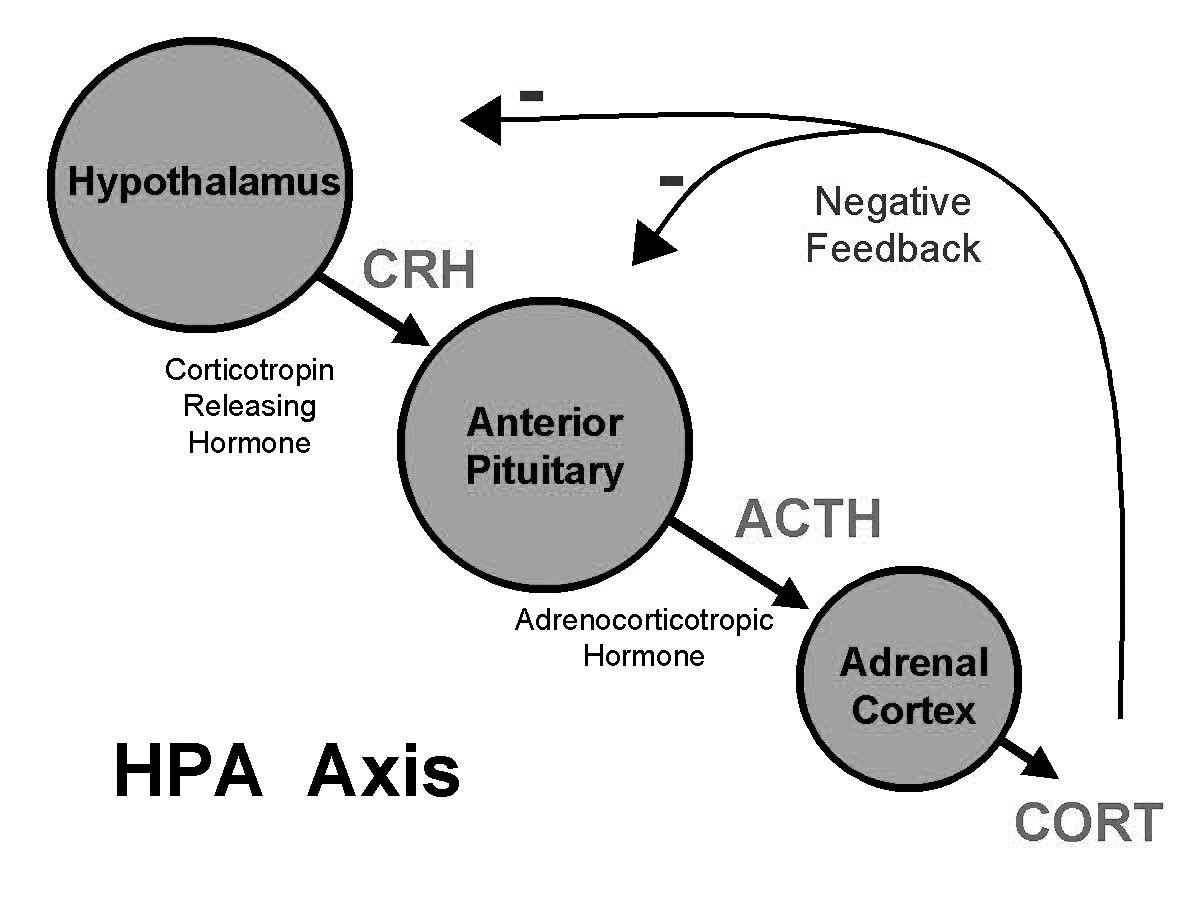
The process of maintaining constancy amidst change is called homeostasis. Homeostasis is coordinated most obviously via the neurotransmitters of the nervous system and the hormones of the endocrine axis. The endocrine axis has correspondences with the chakras of Eastern spiritual disciplines1 but modern Western medicine has simplified this to the HPA (hypothalamus-pituitary-adrenal) Axis. The HPA axis continually assesses what’s happening in the body, gives feedback, and calls for appropriate action, using hormones as its messenger molecules.
Hormones are the messenger molecules that coordinate and direct immediate adjustments, diurnal rhythms and the longer transitions across the stages of life: infancy, childhood, adolescence, maturity, senescence and death. They work in coordination with neurotransmitters.
The key difference between hormones and neurotransmitters is that hormones are generated by specific glands.2 The hormones are conveyed through the bloodstream on protein carrier molecules to their target organs, where they are received by specific cellular receptors.
Neurotransmitters travel essentially as electrical impulses directly from neurons (nerve cells) to other neurons or to muscle cells, usually a shorter distance, moving instantaneously, much more rapidly than hormones, and without particular (or obvious) rhythms.
THE HPA HIERARCHY
The HPA endocrine axis is based on the components that currently get the most attention in Western medicine, and addresses interactions among the hypothalamus, pituitary and adrenal glands. The tissues affected by the endocrine axis comprise all those of the body, in a semi-hierarchical system. In this system, the “general” (the hypothalamus) perceives, oversees and assesses everything going on in the body, then informs its “officer lieutenants” in the pituitary gland. The “officers” in the pituitary gland inform the “sergeants” (the target organs), who then enlist the “troops” (particular biochemical processes) in the relevant tissues or organs in the body. The enlisted or activated tissues include the visceral organs—heart, lungs, intestines, kidneys, liver, pancreas (and their less publicized ancillary agents such as the gallbladder, spleen, blood vessels, etc.)—and the skeletal muscles.
The secretions or hormones from these glands thus have an effect on the entire body and its balance amidst constant input and response—thus maintaining homeostasis. It is an intricate and delicate system of feedback loops and checks and balances, affecting all the cells and tissues of the body, whose operation and processes it maintains both day to day and across the years.
The entirety of the endocrine system comprises the pineal gland, the hypothalamus, the pituitary, the thyroid and parathyroid glands, the thymus, the pancreas, the adrenal glands and the gonads—ovaries in women, testes in men. In this essay, the focus will be on the hypothalamus and the pituitary, and their key agents, the thyroid and adrenal glands, and to a lesser extent, the gonads or reproductive organs.
HOMEOSTASIS
Occupational therapist Maude LeRoux describes beautifully in her book Our Greatest Allies3 the fundamental capacities exhibited by a being newly arrived in this world:
• Vestibular balance—a sense of uprightness or verticality
• A way to modulate the amount of sensory input allowed in
• A way to process what stimuli are allowed beyond one’s outer boundaries.
These are facets of homeostasis, and remind us that when someone doesn’t respond as we might expect, that person’s homeostatic mechanisms, especially the HPA axis, are probably fully occupied and don’t have room for anything more. In other words, it’s not malice; it’s simply a self-preserving physiological response. Often a homeostatic effort by the body is considered a disease or illness, which allopathic medicine commonly seeks to obstruct or eliminate. A more holistic perspective views imbalances such as fever as the body’s efforts to “burn out” some potentially toxic or extraneous substance. Similarly, digestive upsets—vomiting or diarrhea—or skin eruptions like rashes and warts are recognized as efforts to eliminate noxious substances.
In exploring the endocrine axis it can be daunting to keep track of so many terms, many of which seem similar, along with their corresponding abbreviations, and then try to remember their particular functions and the subtle differences and relationships among them! Most of the names are ancient language equivalents, mostly from Latin and Greek, simply meaning “that do-widget which is next to the thing-a-mabob.” The names are descriptions of function or location. Pronunciation, as a wonderful biology prof instructed us decades ago, is usually based on emphasizing the least meaningful syllable of the word.

A disturbance in any of the organs or tissues4 in the HPA or greater endocrine system affects all of the glands of the axis, eventually affecting the entire body. In other words, a thyroid problem is not merely a thyroid problem, nor is adrenal fatigue simply an adrenal issue. An imbalance or malfunction assumed to be simply a disturbance in one area of the body really is a systemic problem, affecting the entire body. A fundamental tenet of therapeutic massage states: “it’s all connected.” While this understanding is fundamental with acupuncturists, neuromuscular therapists and craniosacral therapists, few allopathic medical practitioners take this assumption into consideration.
THE HYPOTHALAMUS
The hypothalamus of the HPA is located centrally in the cranium at the floor of the cerebrum (brain), surrounded by cerebrospinal fluid (CSF) and in close and continuous contact with freshly oxygenated blood from the aorta. It is at the crossroads of the central and peripheral nervous systems (CNS and PNS, respectively), as well as circulatory flow, and thus monitors the most recent changes and conditions throughout the body. Information on external sensory input such as taste, smell, touch, sight and sound, as well as visceral responses arrive at the hypothalamus, apprising it of blood temperature and pH; solute content as osmotic pressure and barometric pressure; general and specific levels of amino acids, mineral levels and balance; and blood sugar (glucose and other) levels, concentrations of insulin and other hormones. In addition, the hypothalamus registers gastric motility, heart rate and contractions of the urinary bladder, along with circadian changes and the transformations of the life cycle. The hypothalamus is indeed the central monitor and control center for the body.
Having assessed everything from both circulatory and nervous systems, the hypothalamus responds accordingly. Based on the information flowing through it, the hypothalamus dispatches individual hormones in two sets to the pituitary. One set inlcudes oxytocin and antidiuretic hormone (ADH). Both are synthesized in the hypothalamus, derived from the same prototypical protein. The two hormones travel, separately, to the posterior pituitary gland (also called the neurohypophysis) for storage, ready for release as directed. They both promote smooth muscle contraction. Oxytocin stimulates uterine contractions, especially important for childbirth, then contracts the mammary glands for milk “let-down.” Oxytocin is known as the “love hormone” because it also promotes instincts for cuddling and nurturing, as well as sexual arousal and orgasm.
ADH also goes by the name AVP or arginine vasopressin. It prompts contraction of the smooth muscles in arterioles and sweat glands, causing them to retain fluid. ADH also prompts the kidneys to retain water. The posterior pituitary releases ADH when blood pressure (BP) is low, and also in times of pain and exposure to drugs such as nicotine, morphine and barbiturates, perhaps providing “dilution as the solution to pollution.” Excessive ADH release in the hypothalamus occurs with severe blood loss, trauma or other injury or abnormal cells such as cancer. Excessive ADH release with consequent excessive water retention is manifest as weight gain, bloating and hypo-osmolality of blood (that is watery blood or too much liquid and not enough minerals, blood cells, carrier molecules with cargo, or other dissolved content).
The other set of hormones from the hypothalamus comprises both releasing and inhibitory hormones. These go from a capillary bed in the hypothalamus, through a vein directly to a capillary bed in the anterior pituitary.5 They do not go through the systemic circulation, nor do they pass through the heart and lungs. They arrive directly at the anterior pituitary (also known as the adenohypophysis), where they convey their instructions to yet another set of hormones, the tropic hormones.
Hypothalamic-releasing hormones include:
• Growth hormone-releasing hormone (GHRH)
• Thyrotropin-releasing hormone (TRH)
• Corticotropin-releasing hormone (CRH)
• Gonadotrophin-releasing hormone (GnRH)
• Prolactin (PRL).
Countering, or putting the brakes on the synthesis and release of tropic hormones from the anterior pituitary, are two additional hormones from the hypothalamus. These are inhibitory hormones:
• Growth hormone inhibiting hormone (GHIH), also called somatostatin
• Prolactin inhibiting hormone (PIH) also called dopamine.
THE PITUITARY
Hormones from the hypothalamus inform the pituitary that there’s work to be done. Tropic hormones from the anterior pituitary then go out into the body to set the appropriate work-response into action.
The pituitary gland was in past years known as the master gland but lost that title as awareness of hypothalamus function increased. Current thinking is that the hypothalamus is the central controlling agent, whose role is to notify the pituitary to send out deputy messengers to the tissues (and the cells of which they are made), which do the actual work.
The pituitary gland rests in the sella turcica (Latin for Turkish saddle), a small indentation in the sphenoid bone. The sphenoid bone is notable because it comes into contact with every other bone of the cranium or skull. The significance of this is that any shift in position of the cranial bones affects the pituitary. Such a positional shift could come from obvious physical trauma like a blow to the head, or from subtle shifts in the fascia.6
Dr. Weston A. Price, in his seminal work, Nutrition and Physical Degeneration,7 noted that vitamin E deficiency produced changes consistent with those of hypophysectomy (surgical removal of the pituitary gland). Down syndrome, prolonged gestation possibly with resorption of the fetus, incomplete calcification of the skull and degranulation of the anterior pituitary are all abnormalities Dr. Price was aware of in connection with vitamin E complex deficiency.
The anterior pituitary synthesizes and releases specific hormones in response to the arrival of releasing, or inhibitory, hormones from the hypothalamus. The anterior pituitary secretes:
• Somatotropins such as growth hormone (GH)
• Corticotropins such as adrenocorticotropic hormone (ACTH)
• Gonadotropins such as follicle-stimulating hormone (FSH) and luteinizing hormone (LH)
• Lactotropins such as prolactin (PRL)
• Melanocyte-stimulating hormone (MSH).
SOMATOTROPINS
Somatotrophs are the most abundant cells in the anterior pituitary. These anterior pituitary cells release somatotropic hormones (somatotropins), particularly GH (growth hormone or hGH for human growth hormone) in response to releasing GHRH from the hypothalamus. GH travels through the bloodstream to the tissues of the body, particularly the liver, skeletal muscle and cartilaginous structures such as fascia, joints and bones. In the pancreas, GH stimulates the release of glucagon, a hormone whose name means “glucose is all gone,” to activate a rise in blood sugar. In other tissues GH elicits synthesis and secretion of IGFs (insulin-like growth factors).
IGFs prompt cells to grow by activating uptake of both the increased glucose in the blood as well as of amino acids and their incorporation as proteins8 into the substance of a tissue. In childhood and adolescence, the effect is to promote growth. In adults, IGFs maintain muscle and bone mass and support tissue repair. In addition, IGFs promote lipolysis, release of fats (lipids) from adipocytes (fat cells), for use as fuel by the cells affected by GH. Interestingly, IGFs decrease uptake of glucose by those affected cells, giving preference to the use of fats for ATP production, sparing the glucose so that it can be used by the neurons (nerve cells) in the brain.9 Perhaps this is a factor in the difference between insulin and IGF.
Insulin is made and secreted by the pancreas in response to elevated blood sugar. Unlike IGFs, which decrease the uptake of glucose by the cells, insulin’s most prominent role is to deliver blood glucose to cells where it is used to generate energy as ATP. Insulin also facilitates entry of amino acids into cells and activates protein synthesis. Insulin is unlike most other hormones in that it is anabolic, that is, it promotes construction of substances, in contrast to catabolic agents which break substances down. Any excess glucose, or protein as amino acids, beyond what can be immediately used for fuel or construction, is either stored as glycogen or as fat.
This is a crucial point. It is not fat that makes a person fat; it is excess carbs. The body converts excess carbohydrates, particularly refined carbohydrates, to fat.
Insulin’s net effect is to lower blood sugar. If blood sugar is chronically and inordinately elevated, after a while the β-cells of the pancreas lose their capacity to secrete insulin and burn out, resulting in diabetes. This happens with constant consumption of refined sugars and starches. Continued fluctuation of blood sugar levels places exhausting demands on homeostasis and the entire hormone axis, and is profoundly stressful. The ensuing disorder then emerges as disease. Simply eliminating the symptoms, either by covering them up or blocking the metabolic pathways that generate them, does not cure the disease nor heal the person. Mere elimination of symptoms perpetuates the endocrine axis disarray, and in effect drives the disease deeper.
In a healthy, properly operating system, as blood levels of glucose rise, feedback to the hypothalamus inhibits GHRH and activates GHIH (that is, somatostatin10). GHIH then instructs the somatotrophic cells of the anterior pituitary to cease producing and secreting GH.
Regulation of both GHRH and GHIH is through blood sugar (glucose) levels, with hyperglycemia inhibiting GHRH—as if to say “Enough already! Don’t promote any more growth!” Hypoglycemia, low blood sugar, by contrast, has an inhibitory or suppressive effect on GHIH, and the net effect is to increase GHRH, hence GH, with consequently increased levels of blood glucose. Chronic or persistent excess of GH leads to constant hyperglycemia or elevated blood sugar. This in turn prompts the pancreas to secrete insulin, since blood sugar levels as well as fluid are closely regulated.
An excess or hypersecretion of GH affects the growth of tissues throughout the body but becomes most evident as excessive growth in the long bones, leading to abnormal height or gigantism, with acromegaly11—enlarged hands, feet and facial bones, coarse features and an enlarged tongue. Insufficient or hyposecretion of GH in children, by contrast, leads to pituitary dwarfism with adult height being about four feet, but with relatively normal proportions. While research is inconclusive, severe deficit of GH in children has been linked with progeria, where body tissues atrophy and accelerated aging ensues.12
Blood sugar as well as fluid content are both closely regulated. Homeostasis, the delicate balance to keep the complexities of the body running smoothly, can easily be disrupted if constant fluctuations and demands are imposed on it. Since GH summons the release of glucose from storage (as glycogen) in the liver and prompts the conversion of some proteins into glucose via gluconeogenesis,13 the current societal excess of dietary sugar is a conspicuous culprit in hormone imbalances and its various manifestations.
THYROTROPINS
TRH (thyrotropin-releasing hormone14) from the hypothalamus stimulates the production and release of TSH by the anterior pituitary. TSH goes via the blood to the thyroid gland, situated in the anterior neck (in front of the throat). TSH then prompts the thyroid gland to make and release thyroxine.
Thyroxine or thyroid hormone (also called T4) is made in the thyroid gland from four molecules of iodine added to tyrosine, an amino acid. T4 is what’s in Synthroid, but this is the inactive form of thryoid hormone. T4 is conveyed through the bloodstream to cells where it is converted to T3 , the active form of thyroxine, to get those cells working.15 In some ways T4 converted to T3 is like an accelerator: its role is to turn the cell’s machinery on. To do that, a specific iodine molecule needs be “chipped” off of the tyrosine template. Under stress, especially elevated cortisol, and other adverse conditions, the “wrong” iodine molecule is removed, leading to rT3, which occupies the site but cannot complete its mission of activating the cells’ functions; in other words, it’s a dud.
TSH is typically the hormone measured when thyroid problems are suspected, but it is only a small part of the whole picture. Elevated TSH means there is inadequate response from the cells when the thyroid summons T4 and T3 to work harder.
Nutrient deficiencies can underlie inadequate response. Tyrosine can be derived from another amino acid, phenylalanine; one or the other must come from the diet, as the body cannot make them from bodily resources. The net effect is that without phenylalanine or tyrosine, the material from which we generate thyroxine is missing. Adequate protein and robust digestive capacity are both necessary to ensure adequate amounts of this important substance. Vitamin A16 has a mutual relationship with iodine for generating thyroxine. In addition to iron and iodine, selenium is a necessary mineral cofactor for thyroid hormone synthesis, activation and metabolism. When TSH is elevated and cells still fail to respond sufficiently, it’s quite likely that selenium is inadequate.
There’s an interesting nexus here. Assuming all other factors are in place, a cell will function as long as it has glutathione, abbreviated GSH, to capture free radicals given off when a cell is actively metabolizing. Glutathione is the body’s major antioxidant, the key agent to capture free radicals or ROS—reactive oxygen species. When a cell operates, it gives off ROS. If a cell continues to operate when it doesn’t have enough GSH, the unfettered ROS “sparks” will cause damage to the cell itself, eventually damaging neighboring cells and tissues as well. Selenium is not only the mineral cofactor necessary to convert T4 to its active T3 form. Selenium is also necessary to produce GSH (glutathione). If it doesn’t have the necessary GSH, the cell either shifts to “emergency generator mode,” so at least it can stumble along until there’s enough GSH to keep it up and running, or it undergoes apoptosis. Apoptosis is deliberate cell death, whereby the cell sacrifices itself, dies and lets its parts be recycled for reuse. By taking damaged cells out of function, the tissue can keep operating (assuming the remaining cells have enough GSH) and not “burn the body” down by giving off unhindered free radicals.
The possible nexus here is that if a cell doesn’t have enough selenium to make the GSH, it probably also does not have enough selenium to convert T4 to active T3. In effect, the body recognizes that if there isn’t enough selenium to make the protective GSH, there’s no point in converting T4 to active T3 because the cells can’t respond anyway.
In addition, when a cell metabolizes fats (as fatty acids) to generate energy as ATP, the process is much more efficient than using glucose or sugar. It’s the difference between generating heat and light from a large log that burns for hours, and depending on scraps and twigs that flash and dissipate in the moment. Fats are also necessary for vitamin A to be absorbed. Again, iodine17 and vitamin A need each other for optimal absorption and use in thyroxine production. One could speculate that when the body recognizes a situation where it doesn’t have all the materials necessary to function well, it doesn’t set itself up for a process it can’t sustain properly.
A complete discussion of thyroid function warrants volumes. Succinctly, when thyroid dysfunction is suspected, because the thyroid gland is part of a complex web of interacting tissues, the problem is not solely in the thyroid. An overall endocrine axis imbalance is highly likely, with autoimmune issues present as well. A complete thyroid panel is necessary to understand where and why the body’s homeostatic efforts are bogging down.18
Additional resources toward understanding the thyroid are listed in the endnotes.19
CORTICOTROPINS
CRH from the hypothalamus stimulates the anterior pituitary to make and release ACTH (adrenocorticotropic hormone, also called corticotropin), which goes to the adrenal glands and elicits a response according to need and receptor sensitivity.
The adrenal glands are small caps atop the kidneys, the name deriving from Latin, meaning “of the kidneys.”20 The adrenal glands have two distinct areas to them. The interior area is closely related to the nervous system and is called the adrenal medulla. The outer part of the adrenal glands is the cortex or “crust.” Corticotropins affect the cortex of the adrenal glands.
The adrenal cortex has three layers. The outermost is the zona glomerulosa. This is related to the glomeruli of the kidneys, from the Latin, “little balls of yarn,” referring to the extensive lengths of fine tubing that filter fluid, minerals and other solutes from the blood to generate urine. The zona glomerulosa has to do with regulating electrolyte and fluid balance. While controlled by ACTH (from the anterior pituitary), it lacks the enzymes21 necessary to provide the same response that ACTH summons from the other layers of the adrenal cortex. Here, in the zona glomerulosa, and only here, the mineralocorticoid aldosterone, is produced.

Aldosterone prompts the kidneys to retain sodium and excrete potassium. It works in conjunction with the renin angiotensin system and other factors, but the key point is that aldosterone prompts the kidneys to reabsorb sodium. Since water follows salt, aldosterone instructs the kidneys to keep the salt and hence the water, too. This maintains blood volume. Blood pressure depends on both the volume of the blood and the tension of the smooth muscles in the blood vessel walls. A rise in either will increase blood pressure.22
Secretion of aldosterone is activated in response to ACTH from the anterior pituitary (responding to CRH from the hypothalamus). Elevated or relatively high plasma (blood) potassium (hyperkalemia) and low blood volume are two factors that activate the release of CRH. Maintaining a proper balance of sodium and potassium is crucial to cell membrane response, hence cell function, thus indispensable for life. A lack of sodium (salt) or aldosterone can be fatal, as can an excess of potassium. The body goes through major and multiple efforts to maintain proper sodium and fluid balance. Both ADH from the hypothalamus and aldosterone from the adrenal’s outer layer, the zona glomerulosa, along with the renin angiotensin system in the kidneys, are constantly active to regulate electrolyte balance.
Licorice (Glycyrrhiza glabra, Glycyrrhiza uralensis) is often recommended for people with apparent adrenal issues. While licorice root can lengthen the time it takes the body to break down cortisol, it can also increase aldosterone levels so much as to severely disrupt the balance of sodium and potassium if ingested in excess.23
Historically, adequate access to salt, along with water, has been a driving force in civilization’s
settlements and battles. Excess salt intake is easily avoided by not consuming processed packaged “foods of
commerce.” An overall vitality-promoting balance of sodium, potassium and other minerals is best obtained through nutrient-dense foods grown in mineral-rich and microbe-rich healthy soil, adding salt to taste as a conscious act.
Symptoms of low aldosterone include:
• Craving salt
• Fluid retention in the arms and legs
• Pupils not staying constricted when exposed to light
• Rough or sandpaper tongue
• Excessive urination up to fifteen or twenty times per day
• Excessive sweating even without activity.
People who crave chips and pretzels, who douse everything with salt, are prime suspects for adrenal problems and HPA or endocrine disruption in general.
The next two layers of the adrenal cortex, the zona fasciculata and zona reticularis, are regulated by ACTH from the anterior pituitary. The zona fasciculata secretes glucocorticoids—essentially cortisol—and the innermost zona reticularis secretes DHEA, androgens and estrogens—the sex hormones. Which hormone is activated depends on the nature of the enzymes present in the particular zone and the presence of other ancillary synergistic agents. In other words, it’s not a simple linear system, but one of complex cooperation and interaction.
All adrenal cortical hormones are generated from cholesterol. The adrenal cortex contains the highest concentration of cholesterol outside the nervous system. The brain is 70 percent lipids, including cholesterol. The adrenal cortex uses cholesterol to synthesize aldosterone, cortisol and DHEA, from which the sex hormones are made.
Cholesterol is so important to health that all tissues of the body24 are capable of generating it. When serum cholesterol is low, the body is severely limited in its capacity to repair and renew itself. Limiting dietary cholesterol intake is futile, since the body will make as much cholesterol as it needs. Conversely, vegetarians or vegans, who argue that consuming cholesterol is not necessary, overlook the metabolic expense to the body of making cholesterol. Resources devoted to generating cholesterol are not available for other important roles, and health suffers. Low serum cholesterol is associated with cancer, depression and suicidal and homicidal tendencies. Dr. Price’s accounts of South Sea highland vegetarian groups cannibalizing their seacoast neighbors if denied access to seafood illustrate this important point.
Cortisol is the major hormone secreted by the adrenal cortex, in a diurnal rhythm. Cortisol levels are highest in the morning, lowest at night, unless the endocrine axis is out of balance, as is the common case of “awake all night and sleepy all day.” Cortisol (hydrocortisone) is a glucocorticoid, meaning a cholesterol molecule enhanced with particular sugar25 molecules, and is crucial for life. Apparently all cells have glucocorticoid receptors, and thus can be activated by cortisol or a derivative to one extent or another.
Yes, cortisol is crucial for life. Its primary role is to ensure blood sugar stability, that is, a reliable energy supply so cells can carry out their specific roles. Cortisol summons stored glucose from glycogen stored in the liver and muscles; at the same time it prevents muscle and adipose tissue from taking up glucose, sparing it for use by the brain and heart.
Even before birth, cortisol is necessary. It provides for the maturation of the surfactant of lungs in fetal development; without it, the newborn infant ends up in respiratory distress. Glucocorticoids, represented here by cortisol, have potent anti-inflammatory and immuno-suppressive properties, and thus are widely used for (temporary) relief of arthritis, dermatitis (eczema and rashes) and autoimmune diseases.
Mental, emotional and physical stress are all registered by the hypothalamus, which then informs the anterior pituitary to awaken the adrenal glands to rouse the particular tissues to action. Stress leads to breakdown of bodily tissues for use as fuel, specifically tissues that are high in collagen, since its main component amino acid, glycine, is readily converted to glucose. The effect is consumption of resources which ideally should be available for self-restoration. Instead those resources are directed to deal with external stimuli, resulting in joint deterioration and loss of collagen bone matrix, precursors to osteoporosis.
The most obvious effects of chronically elevated cortisol are disrupted carbohydrate metabolism—blood sugar imbalance—and impaired immune function. Both engender chronic inflammation, the perfect setup for metabolic syndrome. Metabolic syndrome generally manifests as cardiovascular disease and diabetes, the two biggest health problems in modern western society.
Indicators of adrenal dysfunction, affected by cortisol imbalance, with commentary, are shown on page 20. Please note that many health issues that are attributed to adrenal dysfunction are really whole body imbalances. The hormones of the endocrine system are merely the messengers.
In addition to containing the richest store of cholesterol in the body, the adrenal glands hold the highest concentration of vitamin C complex. The indigenous folk of northern Canada knew this and shared the information with Dr. Price because he, unlike other white men they had encountered, did not “know too much to ask the Indian.”26
Nutrients that support adrenal function thus include cholesterol-rich foods such as eggs, especially their yolks, from both fish and fowl; liver and adrenal glands; and full-fat dairy such as cream, butter and cheese. In addition, foods rich in vitamin C complex27 are important and are found in deeply colored fruits and vegetables, particularly the dark colored fruits of summer. Their antioxidant qualities protect from the intense oxidizing properties of the sun.
GONADOTROPHINS
Gonadotrophic-releasing hormone (GnRH) from the hypothalamus stimulates the anterior pituitary to generate follicle-stimulating hormone (FSH), followed by luteinizing hormone (LH). These travel to the gonads—the reproductive organs in both men and women. FSH stimulates the production of estrogen and follicular development in the ovaries of women. LH then activates the release of the ovum as well as stimulating the production of progesterone—optimistic that the ovum (single egg) will be fertilized and need the differentiating and protective qualities of progesterone. The actions of FSH and LH are coordinated with the ebb and flow of estrogen(s) and progesterone in women’s menstrual cycles.
In men, FSH stimulates the development of spermatozoa,28 and LH stimulates the secretion of testosterone. Testosterone works in concert with FSH to complete spermatogenesis, the maturation of sperm. Testosterone also provides for the development of male secondary sex characteristics such as deepening of the voice, facial hair and increased muscle mass.
In addition to production in the ovaries and testes, respectively, the sex hormones are produced in the third, innermost layer of the adrenal cortex, the zona reticularis. Succinctly, DHEA is a cholesterol-based hormone from which androgens and estrogens are produced. DHEA also has a permissive effect. That is, its presence facilitates the production of neurotransmitters, which affect memory and mood. Neurotransmitter imbalances are more likely to occur when DHEA levels are less than optimal. Also, when DHEA is low, which happens after long bouts of chronic stress, overall resilience and immune response are compromised, and senescence is accelerated.
Androgens comprise androstenedione, testosterone, and its various derivatives such as DHT (dihydrotestosterone, which plays a role in male pattern baldness). Estrogen has at least three forms: estrone, estradiol and estriol. As noted above, each of these has particular functions both in reproduction as well as in day-to-day maintenance of the physical structure—all the changes across the lifetime journey.
Both men and women have some of each of the three major sex hormones29 (and their derivatives, not covered here), in gender-appropriate proportions. Testosterone supports libido and is especially important for maintenance of all types of muscle tissue: skeletal, smooth (lining arteries and glands) and cardiac. Increased risk of cardiac failure (heart attack) occurs with insufficient testosterone. Statin drugs interfere with the production of cholesterol, the key substrate from which testosterone is produced. It should be no surprise that muscle pain (myalgia), weakness (myopathy), and dissolution of tissue (rhabdomyolysis—tissue turning to “jelly”) are well-known side effects of taking statins.
LACTOTROPHINS
In response to GnRH from the hypothalamus, and in conjunction with relatively higher estrogen levels, the anterior pituitary generates and secretes prolactin. Prolactin (PRL) (“for milk” in Latin) activates mammary (breast) tissue to promote milk production; in general it affects reproductive and immune tissue. By itself it has a very weak effect, which makes sense because there is a sequence and relationship among the above hormones. Oral contraceptives, opiates and breastfeeding also all stimulate the release of PRL. In excess, it can be a causative factor in premenstrual breast tenderness. Elevated levels of prolactin may cause amenorrhea—lack of menstrual cycles—appropriate when a woman is nursing a baby, but an indicator of endocrine imbalance when birth and breastfeeding are not in the picture. In men, elevated prolactin is consistent with erectile dysfunction. PRL is inhibited by PIH (prolactin inhibitory hormone, from the hypothalamus), which again makes sense. PIH is dopamine, the get-up-and-go hormone and neurotransmitter. It’s difficult to tend the baby and the home fires when hormones are telling us to go slay dragons or embark on major external efforts.
MELANOCYTE-STIMULATING HORMONE
MSH stimulates the pineal gland to synthesize melanin. Melanin is pigment that gives color to the skin and relates to light exposure with respect to the sun and attunement to the diurnal and seasonal rhythms of light and darkness.
PATTERNS AND CONNECTIONS
It’s easy for a description of the hormones to become massive and overwhelming. Amidst the long, strange, unpronounceable words and complex descriptions, there is actually a pattern to the hormones of the endocrine axis.
GH (growth hormone) enlists IGF (and other substances) to build the physical substance.
TSH (thyroid-stimulating hormone) notifies the thyroid gland to dispatch thyroxine to activate the physical substance, the cells constituting the various component tissues and organs, in effect “turning it on” and in some cases “up.”
Corticotrophs provide support to sustain the organism’s efforts, specifically by ensuring appropriate balance of fluids, minerals and fuel.
Thus established, the organism lines up its successor, making provision for the next generation. FSH and LH prepare the seed and aid its ripening. Prolactin provides nourishment.
Melanocyte-stimulating hormone (MSH) relates back to the top gland of the entire endocrine axis, the pineal gland, furnishing a link with the cosmos beyond the present corporeal and earthly existence. One could say that a living being, having established itself and its offspring on the earth, aligns via MSH and the pineal gland to establish a more extensive connection with the cosmos.
As MSH establishes a connection with the greater cosmos via the pineal gland, it then winds its way through the complexities and subtle distinctions of the endocrine axis to the lowest and “earthiest” set of glands, the gonads, affording humans a role as bridge between the grand scale of existence and the earth. In short, our endocrine system creates a bridge between two worlds.
MOTHER NATURE OBEYED
There is an electromagnetic force between the earth’s surface and the ionosphere, the densest part of earth’s atmosphere, called the Schumann Resonance.30 The Schumann Resonance corresponds to that of alpha brain waves, which resonate at 7.83 Hz, and is said to correspond also to optimal function of the endocrine axis. The Vedic chanting of Om is said to reinforce this frequency, and with it one’s harmonious alignment within oneself (comfortable homeostasis) as well as with the cosmos beyond and the earth beneath our feet.
Obeying Mother Nature entails living with the rhythms and patterns of the earth as a component of a greater cosmic system. My personal take on the adrenals in particular is that their primary role is to allot bodily resources toward self-preservation. In a balanced system, energies are distributed according to the old sailor’s tradition: one hand for the sailor, one hand for the ship. If a person is constantly on the go, expending attention and energy outwardly, responding to external stimuli, and constantly dealing with external stressors and demands, few resources are available to keep one’s internal relationships in harmonious order. The “hand for the sailor” is sacrificed to two hands for the ship and none for the sailor, exhausting the individual with the consequence of lost support for the “ship” or greater endeavor. Adrenal fatigue (or exhaustion or distress) is a sign of overall endocrine dysfunction. Just as humans tend not to thrive in isolation, the tissues and organs of their bodies neither exist nor function in isolation. It is all connected.
A healthy, whole and happy human being is connected with himself or herself through a smoothly flowing endocrine system. That in turn affords vibrant connection with community, as well as via the bridge from cosmos to earth. Resources are balanced between self and the outer world, between “the sailor and the ship.” While adequate nourishment is fundamental to optimal function, living consciously with the world around is also important. One of the best things a person can do to keep one’s endocrine axis flowing smoothly, affording energy for both “the sailor and the ship,” is to take time to rest, relax, be with friends, enjoy the arts, and above all, play.
SIDEBAR
SYMPTOMS OF ADRENAL DYSFUNCTION
• FATIGUE: Cells aren’t getting reliable support for their function.
• SUGAR AND SALT CRAVINGS: “Maybe eating this will give my cells what they are craving!”
• CAFFEINE AND NICOTINE ADDICTIONS: “Please help my body wake up, function, settle down—argh!”
• SLOW MORNING START: “Where’s my coffee?” Sleep time is intended to afford reflection, putting things in order. Get to bed earlier for more effective renewal and restoration.
• LATE AFTERNOON CRASH: “Sweets and cola, or that good old Mountain Dew.”
• BETWEEN-MEAL EATING: Fat sustains; carbs, especially when refined, tantalize.
• DIZZINESS: According to traditional Chinese medicine, dizziness occurs when the liver is overworked, possibly a reflection of chaotic blood sugar fluctuations.
• HEADACHES: The liver isn’t caught up with cleanup from before, so now there are leftovers and clutter to deal with. One interpretation of migraines is that they are spasms due to irregular blood supply to brain tissues.
• ALLERGIES AND ASTHMA: No resources left to deal with strange substances, so just shoo them out as best you can by gasping, coughing, sneezing, sniffling.
• WEAKENED IMMUNE SYSTEM: Too much for the body to deal with; lost track of which “other” substance is helping and which is likely to cause problems.
• INSOMNIA: Can’t fall asleep or can’t stay asleep. Inflammatory reactions spread throughout the body when something is awry.
• DIGESTIVE ISSUES SUCH AS BLOATING AND GAS: At least 70 percent of the immune system is in the gut. If preoccupied with external stimuli, bodily resources just aren’t there to process anything else.
• ULCERS: Even fewer resources are available to balance gut microbes and repair tissues.
• IRRITABILITY: Nerve cells drag or simply quit if they don’t have needed support (such as a consistent fuel supply as steady blood sugar or fats and their derivatives).
• BLURRED VISION: Another indication of irregular and erratic blood delivery of fuel and oxygen.
• MENSTRUAL IRREGULARITIES: Bodily self-preservation takes priority over providing for the next generation.
• GRUMPY-OLD-MAN SYNDROME: Sometimes called male menopause. The priority of self-preservation over
providing for others isn’t gender-specific.
REFERENCES
1. Bayne, Kim. (2016) Your 7 Chakras & the endocrine system. Retrieved 2017-11-19 from http://blog.thewellnessuniverse.com/your-7-chakras-the-endocrine-system/.
2. Glands are small sacks of smooth muscle lined with secretory cells. They release their contents upon specific stimulation, as messengers to themselves (autocrine), neighboring cells (paracrine), to the bloodstream in general (endocrine), or through ducts to another organ, such as pancreatic enzymes to the lumen of the small intestine.
3. LeRoux, Maude, and O’Malley, Lauren. (2012) Our Greatest Allies: Respect, Relationship and Intervention … A Child’s Journey. Fort Collins, CO: A Book’s Mind.
4. Cells are the basic unit of life. Many similar cells constitute a tissue. Several tissues, each of several different types of many cells, make up an organ. The several tissues constituting an organ all support a common purpose or role in the overall system of the organism or living body.
5. Tortora & Derrickson (2009) Anatomy and Physiology, 12th edition. John Wiley & Sons, Inc., p 651.
6. Fascia is the connective tissue enveloping the entire body and all of its organs: smooth and skeletal muscles, the viscera (heart, lungs, kidneys, pancreas, spleen, intestines) and the bones. The fascia attaches to the outer and inner surfaces of the skull, including the meninges, the protective tissues surrounding the brain. Irregularities in the fascia can occur from various causes, including postural habits based on emotional responses or physical behaviors, and tend to be subtle. It is quite possible that the meridians of energy (chi) flow of Traditional Chinese Medicine (TCM) are a reflection of pathways in the fascia. Releasing the various contractions of the fascia through myofascial release, cranio-sacral therapy, or structural integration (aka Rolfing) massage techniques has a distinct effect on a person’s emotional and physical well-being, indeed “changing one’s body about one’s mind.” Because of the pituitary’s location and these connections, such bodywork can be very beneficial toward restoring or optimizing endocrine axis function.
7. Price, Weston A. (2016) Nutrition and Physical Degeneration 8th Edition 23rd Printing. Lemon Grove, CA: Price Pottenger, pp 304-305; 331.
8. Amino acids are the building blocks from which proteins are constructed, or synthesized.
9. Tortora & Derrickson (2009) Anatomy and Physiology 12th edition John Wiley & Sons, Inc., p 653.
10. Somatostatin from Latin: soma – body, and stat – halt or status; as in static, not moving.
11. Acro = end or tip; mega = big, from the Latin.
12. Marieb, E. (1995) Human Anatomy and Physiology 3rd Edition. Redwood City CA: Benjamin Cummings, p 557.
13. Gluco=sugar; neo=new; genesis=generation/production.
14. TRH also stimulates the release of prolactin (PRL) and might serve in addition as a neurotransmitter (via the nervous system, in contrast to travelling through the blood) in regulating wakefulness and loss of appetite.
15. As cells “work” they perform their specific functions as well as give off heat. Thus T3 stimulates both metabolic functions as well as generation of heat. Someone with an overactive thyroid gland is likely to feel warm all the time. Conversely, someone with an underactive thyroid probably constantly feels cold.
16. Vitamin A is a fat soluble retinoid nutrient, not the same as water soluble β-carotene. Retinoid vitamin A can be derived from β-carotene through a long, metabolically expensive process. Conventionally, according to the USDA, vitamin A and β-carotene are deemed to be interchangeable, but that is not a valid premise.
17. The usual recommendation for daily intake of iodine is a mere 150 micrograms. This is in contrast to a recommendation of daily adequate intake (AI) of 0.25 mg for infants, 3-4 mg/day for adults or at least 200 times the amount of iodine. Fluorine is highly toxic specifically to reactions in glycolysis and the citric acid cycle, both crucial metabolic pathways. It is a much more reactive element than iodine, and easily displaces iodine. Without adequate iodine, the thyroid is lost and the rest of the body simply cannot function. In addition to fluorine displacing iodine, bromine is another halide element that displaces iodine and can thus interfere with iodine and thyroid function. Consuming fish and shellfish, along with sea vegetables such as kelp, nori, dulse, digitata, etc. is one of the best ways to ensure adequate iodine intake. For clarity, fluoride (iodide, bromide, chloride, etc.) is the negatively charged ion; fluorine, iodine, bromine. etc. designates the isolated element unbound to anything else, and without an electrical charge, but most eager to find a “partner” for its one unpaired electron.
18. A complete thyroid panel includes:
TSH – Thyroid-stimulating hormone
TT4 – Total thyroxine, both free and bound
FTI – Free thyroxine index
FT4 – Free thyroxine
Resin T3 uptake
Free T3 – free triiodothyronine
r T3 – Reverse T3
When stress is high, the “wrong” iodine is removed, leaving a non-functional rT3, in effect another of the body’s protective measures.
TBG – Thyroid binding globulin
Thyroid Antibodies:
TPO-Ab – Thyroid peroxidase antibodies
TGB-Ab – Thyroglobulin antibodies
Thyroglobulin is the predominant protein in the thyroid gland, and in effect stores both thyroxine and iodine.
19. For further information, see accessible and comprehensive resources on thyroid issues by Datis Kharrazian DHSc, DC; Izabella Wentz PharmD; and Nikolas Hedberg DC.
20. Adrenalin is synonymous with epinephrine. Adrenalin is from the Latin; epinephrine is from the Greek. Epi = above, on top of (apex); nephr = kidney, as in nephron, the functional unit of the kidneys.
21. The zona glomerulosa lacks the enzyme 17-α hydroxylase, which is necessary to synthesize cortisol, androgens, or estrogens. Only the conversion of corticosterone to aldosterone can occur in the zona glomerulosa. Farese, et al. Licorice-Induced Hypermineralocorticoidism (1991) N Engl J Med 1991; 325:1223-1227.
22. Blood volume, peripheral resistance, and cardiac output are the key factors affecting blood pressure. Smooth muscles line the blood vessels; their contraction increases peripheral resistance. Marieb, pp 650-660.
23. Farese, et al. Licorice-Induced Hypermineralocorticoidism (1991) N Engl J Med 1991; 325:1223-1227.
24. The liver generates most of the cholesterol needed by the body, delivering it via LDL carrier molecules in the blood throughout the body. RBCs (red blood cells) lose their mitochondria when they mature. That loss gives them their indented center or squashed shape, and removes their capacity to generate cholesterol.
25. The word sugar commonly refers to white table sugar, sucrose, which is a combination of fructose and glucose. There are many forms of sugar, each a combination of carbon (O), hydrogen (H), and oxygen (O) atoms. They differ by position of at least one O or OH. Position of component atoms determines the structure of a molecule and its function. Specific sugars attached to proteins, fats or cholesterol facilitate functions and biochemical processes unique to that combination.
26. Price, W. A. (2016) Nutrition and Physical Degeneration, 8th Edition, 23rd Printing. Lemon Grove, CA: Price Pottenger, p 69.
27. Vitamin C was discovered in 1912; Albert Szent-Györgi and Walter Norman Haworth received the Nobel Prize for it in 1937. Although Szent- Györgi recognized that it comprised a complex of molecules, political forces insisted it be compressed to ascorbic acid. Common convention thus equates vitamin C with ascorbic acid, while those more attentive to subtle differences recognize vitamin C as a complex of synergistic substances.
28. Spermatozoa are the generative cells produced by men, a single such cell being a spermatozoon. Sperm is the collective term for the spermatozoa, fluid and other substances conveyed in semen.
29. The three key sex hormones are: estrogen – which promotes growth, or “assembly of the basic building materials”; progesterone – calling for differentiation and function-specific application of the assembled building materials; testosterone – supporting muscle function, strength and maintenance. These have to do not only with reproduction of the next generation, but with maintaining the present physical body as well. There are 3 (or more) forms of estrogen and several forms of testosterone. Progestin, used in pharmaceutical products such as contraceptives, is a patentable laboratory substance, alleged to be akin to progesterone. While commonly conflated with, and used interchangeably as a term referring to progesterone, progestin is not progesterone.
This article appeared in Wise Traditions in Food, Farming and the Healing Arts, the quarterly magazine of the Weston A. Price Foundation, Winter 2017.
🖨️ Print post

As someone who has studied physiology for over 40 years (I read and do the questions every time a new Guyton’s Physiology and Lehinger’s Biochem comes out) and practices as both a licensed acupuncturist and a chiropractor and most importantly as a nutritionist; your article is by far the best summary of endocrinology out there.
My guess is you are already aware of Dr. Royal Lee, who both set up a trust fund so Physical Nutrition and Degeneration will be published into eternity, and did much of Dr. Price’s lab work. Your analysis is consistent with his work, which can be read on Selene River Press in the archive section.
As for your article, it is being left in the reception area, and for those patients deemed to be literate enough will receive a copy. Your work is impressive for being succinct, relevant and comprehensive. If you have any additional articles or preferably books you have written, please forward how to get them.
Hello. Can u help me with water retension? Ovaries failed 25 yrs ago. Since then I Battle with lower leg fluid retention. I took birth control, amd then transdermal hormones. Lingered on natural progesterone until 2 yrs ago. Doctor says oh well maybe thats just you. 2 yrs ago took an adaptogen formula, and for the first time all fluid disappeared. Felt awesome. But feeling a little tired, started taking adaptogen with more testosterone effect and now back to square one, plus hair fall (male pattern). Take no medications, eat pretty healthy, yoga, slim build. I do have my share of stress overseeing my 80 yr old mom, and 99 yr old grama in a home. Plus, plus. I have been smoking for 44 yrs. I’m 53.