 🖨️ Print post
🖨️ Print post
Incontinence, whether urinary or fecal, is an embarrassing and not uncommon problem among adults. I became aware of just how frequently it occurs when I attended pelvic physical therapy courses.
At the physical therapy courses, we were assigned the task of going around the room interviewing other course attendees about their bowel and bladder habits so that we could become comfortable discussing these matters. During these conversations, I heard about incontinence in the young (athletes and new mothers), the middle-aged (decreasing estrogen in menopause) and the aged (many reasons).
URINARY INCONTINENCE
Before contemplating abnormal bladder function, it is helpful to consider normal function. Ordinarily, when the bladder is over halfway full, it sends a message to the brain. The brain decides whether this is an appropriate time and place to empty. The bladder is a muscle under autonomic control. The only thing one has to “do” to empty it is to relax the urethral sphincter voluntarily. However, most adults have some degree of pelvic floor dysfunction and find themselves bearing down and tightening the abdominal muscles.
A common bad habit is described with the made-up verb, to “jic.” Those letters stand for “just in case.” For example, before embarking upon the commute to or from work, one visits the bathroom—just in case. In some circumstances, “jiccing” may be a good idea (for instance, at the intermission of the opera). However, “jiccing” day after day is not a good practice because the bladder may not actually be full, meaning that the urine must be forced out.
TYPES AND CAUSES OF BLADDER INCONTINENCE
There are three basic types of bladder incontinence.1 Stress incontinence occurs with coughing, laughing and sneezing and may occur briefly after childbirth, or more permanently at menopause. With urge incontinence (a form of overactive bladder), a strong uncontrollable urge causes the episode. The third type of urinary incontinence, retention or overflow incontinence, occurs when the autonomic innervation to the bladder is damaged and the bladder does not empty completely; when more urine comes from the kidney, there is no room for it, so it “spills out” or overflows.
The two most common reasons for the nerve damage seen in retention incontinence are diabetes and vitamin B12 deficiency. Studies have also reported B12 deficiencies in association with stress incontinence.2
A B12 deficiency can be caused by a vegan diet and by drugs such as proton pump inhibitors (PPIs), which prevent the stomach from absorbing B12 and many other nutrients. Some antidepressants in the selective serotonin reuptake inhibitor (SSRI) class can lead to incontinence by an as-yet poorly understood mechanism.3
Many women suffer from bladder prolapse related to childbirth trauma. Symptoms may arise years after experiencing childbirth and are often exacerbated by the loss of estrogen in menopause. When men have incontinence issues, the problem most commonly follows prostate surgery, but it can also arise with old age, diabetes or vitamin B12 deficiency.
PELVIC FLOOR STRENGTHENING
Exercises to strengthen the muscles of the pelvic floor are a frequently indicated intervention that will help with all types of incontinence—although in retention incontinence, it is also important to identify the reason for the autonomic nerve dysfunction. Unfortunately, physical therapists are not taught pelvic treatments in their training. Those who have made it their specialty have done so by taking extra postgraduate courses.
There are two main approaches to pelvic floor strengthening. The first is the Kegel exercise, which is often accompanied by biofeedback. Most postgraduate courses taken by physical therapists (including the ones that I have taken) teach the Kegel-plus-biofeedback method only. The Kegel exercise may be explained by imagining one is about to pass gas or wet one’s pants and then tightening the pelvic muscles to prevent that from happening. The biofeedback component uses either an internal electrode or surface electromyography (EMG) electrodes taped around the anus. The patient can watch the state of his or her contractions on a monitor.
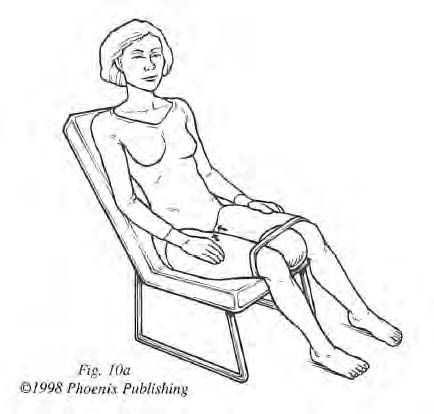
The second approach—exercises developed by physical therapist Janet Hulme—is named “roll for control” (Figure 1). Janet Hulme describes her home programs in Beyond Kegels4 (written for women) and Men After 50: Now What? for men.5 It is fine for an individual to use both methods (Kegel and “roll for control” exercises) concurrently.
I learned about Hulme and her program at a Wise Traditions conference. After ascertaining from Hulme’s website that she was close to sixty-five years old and planning to teach a course in Chicago, I decided I had better attend it in case she was going to retire. Since then, I have taught Hulme’s approach to incontinence to many people. I actually prefer it because it recognizes that the pelvic floor is strengthened by walking and that walking is a natural way of supporting the pelvic floor. Indeed, Janet Hulme says it is common for older people entering a facility to become incontinent in four months’ time, the cause being too much sitting. Some individuals find their gait improved from the Hulme exercises and may no longer need their canes. (Hulme’s books can be ordered at the Phoenix Core Solutions website; both books provide complete, detailed instructions on her home programs.6 Because men are often uninformed about or uninterested in health matters, Hulme’s book for men explains the whole issue in a down-to-earth and practical way.)
For women who suffer from prolapse related to childbirth trauma, performing the Hulme exercises with the hips elevated on an inflatable wedge is beneficial, as shown in Figure 2. (Hulme calls her wedge the “Wonder Wedge.”)6 Conversely, anything that increases downward pressure on the pelvic organs will make things worse. Exercises such as crunches and sit-ups should be avoided. Instead, abdominal strengthening is best performed lying on the floor with the feet elevated against a wall and the hips supported by the wedge.
FECAL INCONTINENCE
Fecal incontinence is another inconvenient and embarrassing problem for many. For women, a common situation is to have suffered a third- or fourth-degree obstetrical tear in childbirth many years previously. At the time, women’s recovery may have been aided by plenty of estrogen. However, when estrogen levels fall at menopause, the traumatized tissues sag, leaving one with fecal incontinence.7 The same exercises used for urinary incontinence are helpful for fecal incontinence.
Diarrhea from any cause will complicate the problem of fecal incontinence. The GAPS (Gut and Psychology Syndrome) diet is well known as a dietary solution for addressing diarrhea.8 However, many of these patients suffer from irritable bowel syndrome (IBS), which not only makes diarrhea unpredictable but can be aggravated by the FODMAPS (short-chain carbohydrates) present in the GAPS diet. We now know that IBS is often related to small intestinal bacterial overgrowth (SIBO), and for this reason a low-FODMAPS diet may be helpful. I have recommended the GAPS diet combined with low FODMAPS for such patients.

MAGNETIC THERAPIES
While researching this article, I became aware of several magnetic treatments for incontinence. I do not have personal experience using these modalities, but I mention them because they are noninvasive, unlike many urologic procedures.
Women’s health specialist and author Dr. Susan Lark recommends the NeoControl magnetic therapy system. Sitting in a comfortable chair, patients experience “powerful pulsing magnetic fields to stimulate nerve activity in the pelvic floor, which in turn exercises the muscles that control bladder function.”9 Typically, the patient has two twenty-minute treatments per week for about eight weeks.
Another magnetic therapy option is Pulsed Electromagnetic Field Therapy (PEMF), approved in the U.S. by the Food and Drug Administration (FDA) for use in urinary incontinence since 1998. One study found improvement in 75 percent of incontinent patients after eighteen sessions of PEMF.10 The Center for Holistic Medicine in West Bloomfield, Michigan uses pulsating magnetic field therapy (PMFT) for one hour twice a week for four weeks, and I am told this therapy has been effective for many people.
NUTRITIONAL CONSIDERATIONS
Dietary triggers may be an issue for urge incontinence and overactive bladder. These triggers are basically the same as those linked to painful conditions such as pelvic pain, painful bladder and interstitial cystitis (a type of chronic pain that affects the bladder). They could be acidic foods, spicy foods and foods containing high amines or glutamates. The approach to take with a suspected food is to eliminate it and then challenge it. If improvement occurs while the food is removed from the diet, then try to establish a threshold of how much can be tolerated without reacting. (Many of these reactive foods are very nutritious, and being able to consume a little of a reactive food can make the diet less restrictive.)
There is anecdotal evidence linking one particular food additive to incontinence, namely calcium propionate, which is added to bread to prevent mold. Calcium propionate may also contribute to bedwetting in children. It is worth eliminating, as there are no good reasons for consuming it.

PREVENTION IS THE BEST MEDICINE
There are several steps one can take to forestall problems down the road. For women who are planning to have children, it helps to be in good condition for childbirth, which will make severe tearing and future incontinence less likely. Third- and fourth-degree obstetrical tears have ramifications later in the mother’s life (just as c-sections have ramifications for the baby’s microbiome). As we age, it also can be useful to have our vitamin B12 levels checked. Know, however, that the “normal” values given by most laboratories are far too low, making it likely that an uninformed doctor will miss this deficiency. Optimal values are at least five hundred picograms per milliliter (pg/mL). Third, it is important to manage blood sugar to avoid diabetes and/or diabetic complications. Finally, if you are dealing with incontinence, know that even if nobody talks about incontinence, you have plenty of company!
SIDEBAR
MEDICATIONS USED IN THE TREATMENT OF URINARY INCONTINENCE AND THEIR SIDE EFFECTS
Pharmacological treatments for urge and retention incontinence act upon the autonomic nervous system either to inhibit or promote bladder emptying. However, even though it would seem quite simple to distinguish between urge and retention incontinence, it is not. Both types of bladder incontinence involve the symptom of continually feeling the need to empty one’s bladder.
With urge incontinence, the bladder nerves are too easily excited—whether the bladder is full or not—whereas with retention, the bladder feels full because it actually is full. Because of this confusion, it is not unheard of for a doctor to prescribe exactly the wrong drug, aggravating the problem. (A urologist can clarify this immediately by performing a bladder ultrasound.)
There are two drug approaches used to treat overactive bladder and urge incontinence. The first blocks the autonomic innervation of the bladder with an anticholinergic agent such as oxybutynin or Detrol. Unfortunately, this class of drugs has a drying effect throughout the body, resulting in symptoms such as dry mouth and constipation.
Conversely, one could stimulate the adrenergic nervous system with a beta-adrenergic agonist. The only drugs of this class for this purpose are Mirabegron or Myrbetriq. However, these come with side effects such as nasal congestion and a transient rise in blood pressure.
Men with prostate enlargement may have difficulty emptying the bladder completely because of obstruction rather than nerve damage. In this situation, a health care provider may prescribe Flomax, an alpha-adrenergic blocker. One side effect of Flomax is a decrease in blood pressure.
Overflow incontinence does not really have a drug treatment. Instead, one might address the patient’s vitamin B12 deficiency, diabetic complications or an underlying neurological condition such as Parkinson’s disease or multiple sclerosis—which could be accompanied by more than one type of incontinence.
REFERENCES
1. Padmanabhan P, Dmochowski R. Urinary incontinence in women: a comprehensive review of the pathophysiology, diagnosis and treatment. Minerva Ginecol 2014;66(5):469-478.
2. Dallosso H, Matthews R, McGrother C, Donaldson M. Diet as a risk factor for the development of stress urinary incontinence: a longitudinal study in women. Eur J Clin Nutr 2004;58(6):920-926.
3. Thurmann PA. [Influence of drugs on urological diseases]. [Article in German]. Urologe A 2016;55(3):401-409.
4. Hulme JA. Beyond Kegels: Fabulous Four Exercises and More…to Prevent and Treat Incontinence, 3rd edition. Helena, MT: Phoenix Publishing; 2008.
5. Hulme JA. Men After 50: Now What? A Handbook for Self-Care and Treatment. Helena, MT: Phoenix Publishing; 2013.
6. http://www.phoenixcore.com/.
7. Fitzpatrick M, O’Herlihy C. The effects of labour and delivery on the pelvic floor. Best Pract Res Clin Obstet Gynaecol 2001;15(1):63-79.
8. Campbell-McBride N. Gut and Psychology Syndrome: Natural Treatment for Autism, Dyspraxia, ADD, Dyslexia, ADHD, Depression, Schizophrenia (revised and expanded edition). Cambridge, UK: Medinform Publishing; 2010.
9. http://www.neocontrol.com/patients/about_neocontrol/neocontrol_facts.htm.
10. Aragona SE, Mereghetti G, Lotti J, Vosa A, Lotti T, Canavesi E. Electromagnetic field in control tissue regeneration, pelvic pain, neuro-inflammation and modulation of non-neuronal cells. J Biol Regul Homeost Agents 2017;31(2 suppl 2):219-225.
This article appeared in Wise Traditions in Food, Farming and the Healing Arts, the quarterly magazine of the Weston A. Price Foundation, Fall 2018.
🖨️ Print post

How long do you squeeze the ball while turning heels in & out?